When you're pregnant, even a simple headache or fever can feel like a crisis. You don’t want to risk your baby’s health, but you also can’t ignore how awful you feel. The question isn’t just acetaminophen pregnancy safety - it’s which pain reliever is truly safe, when, and why. And the answer isn’t as simple as "avoid everything."
Acetaminophen: The Only Go-To for All Three Trimesters
Acetaminophen - also known as paracetamol - is the only over-the-counter painkiller recommended for use throughout pregnancy. It’s been used by millions of pregnant people since the 1950s, and decades of research back its safety when taken correctly.
At standard doses - 325 to 1,000 mg every 4 to 6 hours, not exceeding 4,000 mg in a day - acetaminophen doesn’t increase the risk of birth defects, miscarriage, or developmental problems. A 2023 study of nearly 100,000 mother-child pairs found no link between acetaminophen use and autism, ADHD, or lower IQ scores in children. The adjusted odds ratios were nearly 1.0 - meaning no meaningful difference compared to those who didn’t take it.
It’s not just about pain. Fever during pregnancy is dangerous. A temperature above 100.4°F in the first trimester raises miscarriage risk by 1.5 times. A fever over 102°F can double the chance of neural tube defects. Acetaminophen works fast to bring down fever and reduce inflammation without affecting blood clotting or fetal circulation like NSAIDs do.
Doctors don’t recommend it because it’s "safe enough" - they recommend it because it’s the only option that’s proven safe across all trimesters. The American College of Obstetricians and Gynecologists (ACOG), the Society for Maternal-Fetal Medicine, and the American Academy of Pediatrics all agree: if you need relief, acetaminophen is your best and safest bet.
NSAIDs: The Hidden Danger After 20 Weeks
NSAIDs - like ibuprofen (Advil, Motrin), naproxen (Aleve), and diclofenac (Voltaren) - might seem like a good alternative. They’re strong, widely available, and work well for cramps, back pain, and headaches. But here’s the catch: after 20 weeks of pregnancy, they become risky.
In October 2020, the FDA updated its warning: NSAIDs must be avoided starting at 20 weeks gestation. Why? Because they can cause serious fetal kidney problems. Within 48 to 72 hours of exposure, the baby’s kidneys may stop producing enough amniotic fluid. This condition - called oligohydramnios - can lead to lung underdevelopment, limb contractures, and even stillbirth.
Studies show that 1 to 2% of fetuses exposed to NSAIDs after 20 weeks develop oligohydramnios. That’s 10 to 20 times higher than in unexposed pregnancies. And if you’re past 30 weeks, there’s another risk: NSAIDs can cause the fetal ductus arteriosus - a critical blood vessel - to close prematurely. This can trigger heart failure in the baby.
Even worse, many OTC cold and flu medicines contain NSAIDs. A 2023 FDA review found that 30% of these products don’t clearly label their NSAID content. You might think you’re taking just a decongestant - but you’re unknowingly giving your baby a drug that could harm its kidneys.
There’s no safe window after 20 weeks. Some providers used to say "avoid after 30 weeks," but that’s outdated. The FDA’s 20-week cutoff isn’t arbitrary - it’s based on when fetal kidney development becomes vulnerable. If you took an NSAID between 20 and 30 weeks, your provider may recommend an ultrasound to check amniotic fluid levels. If fluid is low, stop immediately.
What About Low-Dose Aspirin?
Not all NSAIDs are treated the same. Low-dose aspirin (81 mg) is still recommended for pregnant people at risk of preeclampsia. This isn’t a painkiller - it’s a preventive treatment, prescribed by a doctor to improve placental blood flow. The FDA’s warning specifically excludes this use. If your provider prescribed it, keep taking it. Don’t confuse it with regular ibuprofen or naproxen.

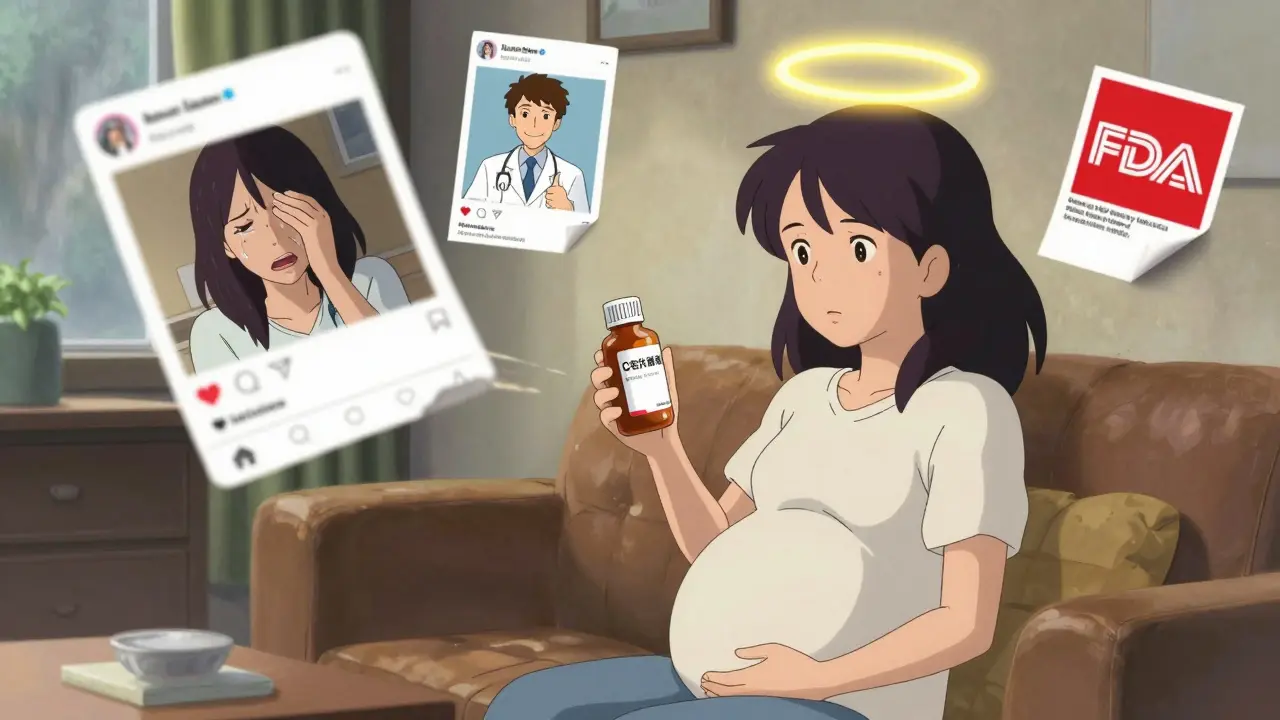
Why So Much Confusion Among Pregnant People?
Despite clear guidelines, many pregnant people avoid acetaminophen entirely. A 2023 survey of 1,200 pregnant patients found 42% avoided it because of rumors linking it to autism. But correlation isn’t causation. The studies that raised concerns looked at long-term, high-dose use - not occasional, short-term use for fever or pain.
One 2021 consensus paper from 14 international experts suggested pregnant people "forego acetaminophen unless medically indicated." But that was a theoretical caution, not a clinical recommendation. Since then, ACOG, SMFM, and the FDA have all reaffirmed acetaminophen’s safety. Dr. Salena Zanotti, an OB/GYN at Cleveland Clinic, puts it bluntly: "Acetaminophen is still the safest known drug to take during pregnancy for problems like fever and pain. It’s OK to turn to medication for help when symptoms are making your daily life difficult."
Meanwhile, social media amplifies fear. Reddit threads and Facebook groups are full of stories about women who stopped acetaminophen because of a viral post - only to suffer through days of uncontrolled fever or migraines. That’s not bravery. That’s risk-taking without benefit.
How to Use Acetaminophen Safely
Even safe drugs need smart use. Here’s how to use acetaminophen the right way:
- Start with the lowest effective dose - 500 mg is often enough for mild pain or fever.
- Take it every 4 to 6 hours as needed, but don’t exceed 4,000 mg in 24 hours.
- Don’t use it for more than 3 to 5 days in a row without checking with your provider.
- Read every OTC label. Many combination products (cold, flu, sleep aids) contain acetaminophen. Don’t double up.
- Keep a log: write down what you took, when, and why. This helps your provider spot patterns.
If you’re unsure whether a medication is safe, bring the bottle to your appointment. Don’t guess. Your provider can check the ingredients and tell you exactly what’s in it.
What If You Accidentally Took an NSAID?
If you took ibuprofen or naproxen once before you knew you were past 20 weeks, don’t panic. One dose is unlikely to cause harm. But if you took it for more than 48 hours, or if you’re unsure how long you’ve been taking it, call your provider. They may schedule an ultrasound to check amniotic fluid levels.
If you’re under 20 weeks and need NSAIDs for a short time - say, for a severe sprain or dental pain - talk to your provider first. They may recommend the lowest possible dose for the shortest time. But even then, acetaminophen is still the better choice.
The Bigger Picture: Pain Isn’t Just a Symptom - It’s a Risk
Some people believe that avoiding all medication during pregnancy is the safest path. But untreated pain and fever carry real dangers. Chronic pain increases stress hormones, which can raise blood pressure and affect fetal growth. High fever can damage developing organs. In some cases, not treating pain is more dangerous than treating it.
ACOG’s president, Dr. Steven J. Fleischman, says it best: "The conditions people use acetaminophen to treat during pregnancy are far more dangerous than any theoretical risks and can create severe morbidity and mortality for the pregnant person and the fetus."
Medication isn’t the enemy. Ignorance is. The goal isn’t to avoid all drugs - it’s to use the right one, at the right time, in the right way.
What’s Changing in 2026?
The science is still evolving. The NIH is running the Acetaminophen Birth Cohort Study - tracking 10,000 children born to mothers who took acetaminophen during pregnancy. Results won’t be in until 2027, but so far, no red flags have emerged.
Some researchers are looking at genetics. A 2024 study found that 15% of pregnant women carry a gene variant (CYP2E1) that affects how quickly their body breaks down acetaminophen. This could mean some people need lower doses. But we’re not at the point of routine testing yet.
Regulators are tightening labels. Since January 2021, U.S. manufacturers have been required to include the 20-week NSAID warning on packaging. But 38% of combination products still don’t comply. That’s why reading labels matters - even more now than ever.
Europe followed the U.S. in 2021 with similar warnings. Australia, Canada, and New Zealand all align with the 20-week cutoff. This isn’t a U.S.-only rule - it’s global consensus.
Is acetaminophen safe in the first trimester?
Yes. Acetaminophen is the only over-the-counter pain reliever recommended for use in all three trimesters, including the first. It’s especially important for treating fever, which can increase the risk of neural tube defects if left untreated. Use the lowest effective dose for the shortest time needed.
Can I take ibuprofen while pregnant?
Avoid ibuprofen after 20 weeks of pregnancy. Before 20 weeks, it may be used occasionally under a doctor’s guidance, but acetaminophen is still the safer choice. After 20 weeks, ibuprofen can cause fetal kidney problems and low amniotic fluid, which can lead to serious complications.
What’s the difference between acetaminophen and NSAIDs?
Acetaminophen reduces pain and fever without affecting inflammation or blood clotting. NSAIDs reduce pain, fever, and inflammation but can interfere with fetal kidney function and blood vessel development after 20 weeks. That’s why acetaminophen is the only one recommended throughout pregnancy.
Is it safe to take acetaminophen every day during pregnancy?
Occasional use is safe. Daily use for more than a few days should be discussed with your provider. While no direct link to developmental issues has been proven, long-term, high-dose use is still being studied. If you need daily pain relief, your provider can help identify the cause and explore non-medication options like physical therapy or heat therapy.
Can I use topical NSAIDs like Voltaren gel during pregnancy?
Topical NSAIDs are absorbed through the skin, but the amount entering your bloodstream is much lower than oral versions. Still, the FDA’s warning applies to all NSAIDs - including gels - after 20 weeks. To be safe, stick with acetaminophen or ask your provider for alternatives like warm compresses or physical therapy.
What should I do if I’m already taking NSAIDs regularly?
Stop taking them immediately if you’re past 20 weeks and call your provider. If you’re under 20 weeks, don’t panic - but switch to acetaminophen and talk to your provider about why you’ve been relying on NSAIDs. There may be an underlying issue - like chronic pain or inflammation - that needs a different approach.
Final Takeaway: Don’t Fear Medication - Fear Uncontrolled Symptoms
You don’t have to suffer through headaches, fevers, or back pain while pregnant. Acetaminophen is your ally. NSAIDs are a hazard after 20 weeks. The key isn’t to avoid all drugs - it’s to choose the right one, use it wisely, and never assume a medication is safe just because it’s "over the counter."
Read labels. Ask questions. Trust your provider. And remember: treating your pain isn’t selfish - it’s necessary for your baby’s health too.