NTI Drug Risk Assessment Tool
Medication Risk Assessment
This tool helps you understand your personal risk level for medication dosing complications based on key health factors. For NTI drugs like warfarin, digoxin, or lithium, even small dosing errors can be dangerous.
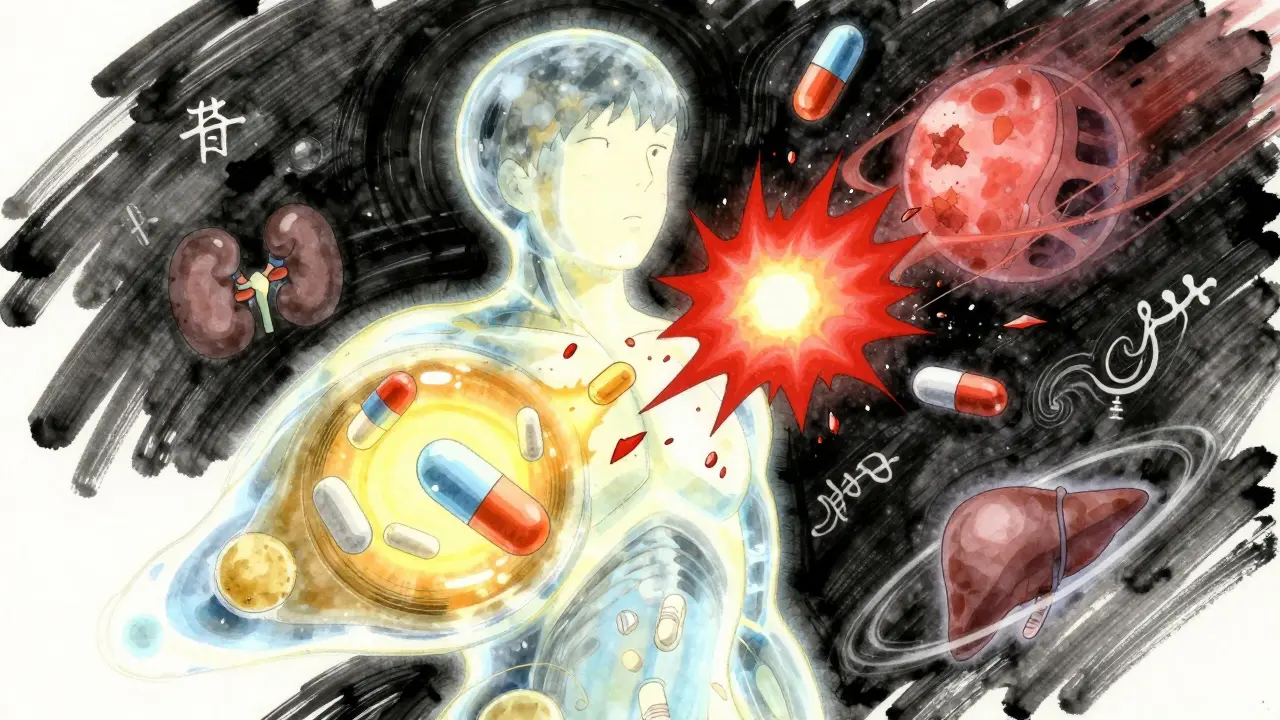
Getting the right dose of medication isn’t just about following the label. It’s about finding the sweet spot where the drug works well enough to help you-without pushing you into danger. Too little, and your condition doesn’t improve. Too much, and you risk serious side effects, hospital visits, or even death. This isn’t theoretical. For drugs like warfarin, digoxin, or phenytoin, a small miscalculation can be deadly. And yet, most people are handed a standard dose and told to take it as-is. That’s not enough.
Why One Size Doesn’t Fit All
Medications don’t act the same in every body. Your age, weight, kidney function, liver health, and even your genes change how your body handles a drug. A 70-year-old with reduced kidney function needs less of a drug than a healthy 30-year-old. Someone who weighs 120 pounds won’t need the same dose as someone who weighs 220. And if you’re taking five other medications, those can interact in ways that boost or block the drug’s effect-sometimes without you even knowing.This is especially true for Narrow Therapeutic Index (NTI) drugs. These are medications where the difference between a helpful dose and a toxic one is razor-thin. Digoxin, used for heart rhythm problems, has a therapeutic index of just 2-3. That means if you take two and a half times the normal dose, half of people could die. Warfarin, a blood thinner, needs constant monitoring because even a slight change in diet or another drug can push your levels into danger. These aren’t rare drugs-they’re commonly prescribed.
What Makes a Drug High-Risk?
Not all drugs need careful tuning. Penicillin? You can take a little more or less without much risk. But NTI drugs like:- Warfarin (blood thinner)
- Digoxin (heart medication)
- Phenytoin (seizure control)
- Lithium (mood stabilizer)
- Cyclosporine (transplant rejection)
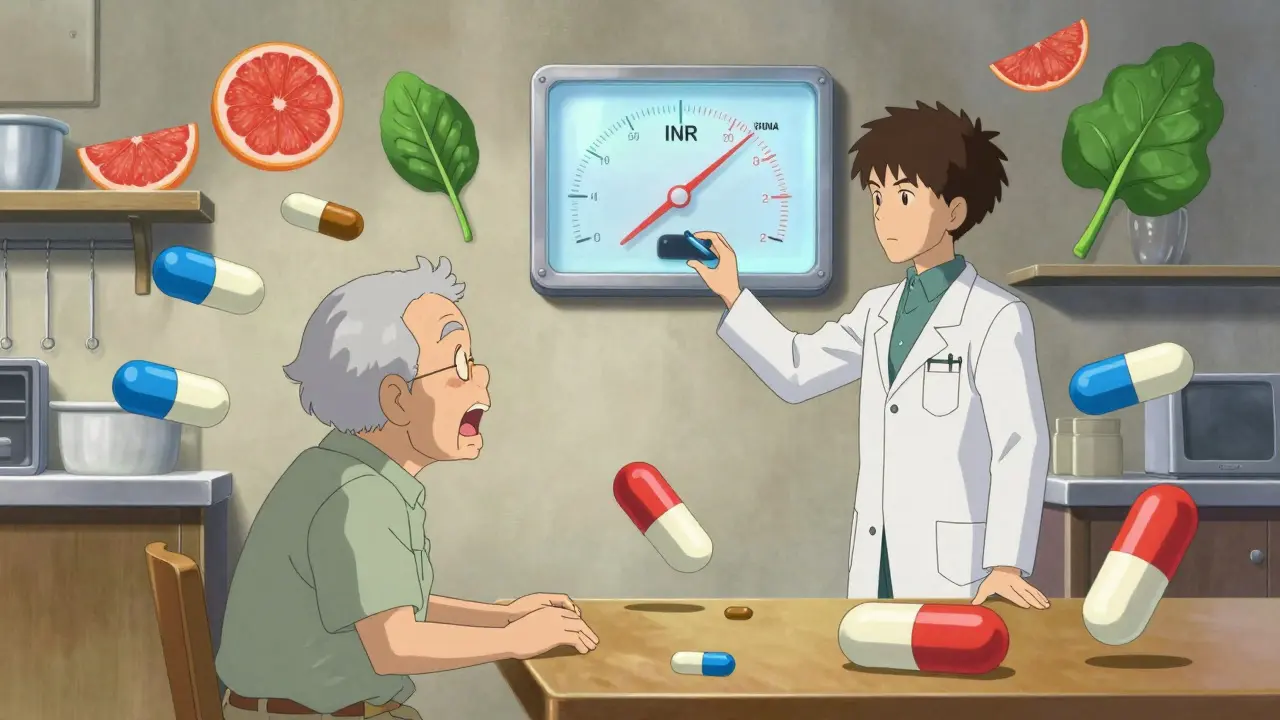
require precision. These drugs are often monitored with blood tests. For warfarin, that’s the INR test-checking if your blood clots at the right speed. For digoxin, it’s measuring the actual drug level in your blood. If your levels are too high, you get nausea, confusion, or dangerous heart rhythms. Too low, and the drug doesn’t work. That’s why regular blood tests aren’t optional-they’re life-saving.
Who Needs Extra Attention?
Some people are at higher risk simply because of who they are:- Older adults: Kidney and liver function decline with age. Many seniors need 20-30% lower doses, but doctors often don’t adjust.
- People with kidney or liver disease: These organs clear drugs from your body. If they’re not working well, drugs build up. Creatinine clearance tests help figure out how much to reduce.
- People taking multiple drugs: Over 44% of adults over 65 take five or more medications. That’s called polypharmacy-and it triples your risk of bad reactions.
- People with unusual body weight: Dosing for obesity isn’t straightforward. You don’t just use total weight. Doctors often use ideal body weight plus 40% of excess weight to calculate doses.
- Those with genetic differences: About 25% of commonly used drugs are affected by gene variations. For example, some people metabolize codeine too fast (risking overdose) or too slow (getting no pain relief).
Here’s the problem: clinical trials rarely include these groups. Most studies test drugs on healthy, middle-aged adults. So when you’re elderly, pregnant, or have complex health issues, your dose is often based on guesswork.
How Dose Adjustments Actually Work
Adjusting a dose isn’t random. It’s a step-by-step process:- Start low: Especially for older adults or those with organ issues. Begin with a lower dose than standard.
- Monitor closely: For NTI drugs, check blood levels or markers like INR every 2-4 weeks until stable.
- Watch for side effects: Nausea, dizziness, confusion, unusual bleeding, or irregular heartbeat are red flags.
- Adjust slowly: Never change a dose by more than 25% at a time. Give your body time to respond.
- Re-evaluate regularly: Your needs change. A new illness, weight loss, or starting a new drug can mean your old dose is now wrong.
Pharmacists play a huge role here. They’re trained to spot interactions, calculate doses based on kidney function, and catch when a patient’s regimen is getting too complicated. In hospitals with pharmacist-led anticoagulation clinics, major bleeding events from warfarin dropped by 60%.
What to Do If You’re on a High-Risk Drug
If you’re taking warfarin, digoxin, lithium, or any NTI drug:- Keep a written list of all your medications-including vitamins and supplements.
- Ask your doctor or pharmacist: “Is this a narrow therapeutic index drug? Do I need blood tests?”
- Know your target range. For warfarin, INR should be 2.0-3.0. For digoxin, blood levels should be 0.5-2.0 ng/mL.
- Don’t skip doses or double up if you miss one. Call your provider instead.
- Be careful with food. Grapefruit can interfere with many drugs. High potassium foods (bananas, spinach) can affect digoxin.
- Use a pill organizer-but don’t rely on it alone. Check labels every time.
And if you’re confused? Ask for a medication review. Many clinics offer free, one-on-one sessions with pharmacists to go over your entire list. These reduce errors by 35% and cut hospital visits by 22% in older adults.

The Bigger Picture: Why This Matters
The drug industry often sets doses based on what worked in clinical trials-not what works for real people. A 2023 study found that many patients are stuck on doses that are too high, simply because guidelines haven’t caught up. Higher doses don’t always mean better results. For statins, the extra benefit from high doses is tiny, but the risk of muscle pain, liver damage, or diabetes goes up.And cost? Drug companies price based on what the market will bear-not what’s safest. That means you’re often paying more for a higher dose that doesn’t help-and might hurt.
That’s why personalized dosing is the future. Tools using AI and real-world data are starting to predict the right dose for you based on your age, weight, genetics, and other meds. Some hospitals already use software that pulls in your lab results and automatically suggests a dose. These aren’t sci-fi-they’re here, and they’re working.
What You Can Do Today
You don’t need to wait for high-tech solutions. Start now:- Ask your doctor: “Is my dose right for me-not just for the average person?”
- Request a medication review with your pharmacist. Bring your full list.
- Track your symptoms. Note when you feel worse or better after a dose change.
- If you’re on an NTI drug, ask about monitoring. Don’t assume it’s being done.
- Deprescribe. If you’re on five or more meds, ask: “Which ones can I stop?” Reducing pill burden cuts risk fast.
Medication isn’t a set-it-and-forget-it tool. It’s a tool that needs tuning-like a car engine. You wouldn’t drive with the wrong fuel mix. Don’t take drugs that way either. Your body is unique. Your dose should be too.
What is a Narrow Therapeutic Index (NTI) drug?
An NTI drug is one where the difference between a safe, effective dose and a toxic or deadly dose is very small-usually a ratio of 2 to 3 or less. Examples include warfarin, digoxin, lithium, and phenytoin. Even small changes in dose or how your body processes the drug can lead to serious harm or death. These drugs require close monitoring, often with blood tests, to stay in the safe range.
How do I know if my medication needs dose adjustment?
If you’re taking a drug like warfarin, digoxin, lithium, or phenytoin, yes-it almost certainly does. Also, if you’re over 65, have kidney or liver disease, are underweight or obese, or take five or more medications, you’re at higher risk for needing an adjusted dose. Ask your doctor or pharmacist: “Is this a narrow therapeutic index drug? Do I need regular blood tests?” If you’re unsure, get a medication review.
Can I adjust my own medication dose?
Never. Even small changes can be dangerous, especially with NTI drugs. Missing a dose or doubling up can cause serious harm. If you think your dose is too high or too low, talk to your doctor or pharmacist. They can check your blood levels, review your symptoms, and make a safe change. Self-adjusting is a leading cause of preventable hospitalizations.
Why do I need blood tests for some medications?
Blood tests measure how much of the drug is in your system. For drugs like warfarin or digoxin, the goal isn’t just to take the pill-it’s to keep the level in your blood exactly where it needs to be. Too low, and it doesn’t work. Too high, and it’s toxic. These tests tell your doctor whether your current dose is right for you right now-not just what the label says.
What should I do if I experience side effects?
Write down exactly what you’re feeling, when it started, and if it’s linked to taking your medicine. Then call your doctor or pharmacist. Don’t wait. For NTI drugs, side effects like dizziness, nausea, irregular heartbeat, confusion, or unusual bleeding can mean your dose is too high. Don’t stop the drug unless told to-just get help. Your provider may need to adjust your dose, check your blood levels, or switch you to a safer alternative.
Can my diet affect my medication dose?
Yes, especially with drugs like warfarin and digoxin. Warfarin works differently if your vitamin K intake changes-so eating lots of spinach or kale one week and none the next can throw off your INR. Digoxin levels rise if your potassium drops, which can happen with diuretics or low-potassium diets. Grapefruit juice can interfere with many drugs by blocking how your liver breaks them down. Always ask your pharmacist: “Are there foods or drinks I should avoid?”
What if I’m taking five or more medications?
You’re at triple the risk of harmful side effects. This is called polypharmacy. The first step is to ask your doctor: “Which of these medications are still necessary?” Many people are on drugs they no longer need-like a statin they started years ago, or an old painkiller. A medication review with a pharmacist can cut your pill count, reduce side effects, and save money. Don’t assume everything on your list is still needed.