When your body turns on itself, life doesn’t pause for a bad day. For people with autoimmune diseases, a flare isn’t just a bad day-it’s a full-system shutdown. Fatigue so deep it feels like gravity doubled. Joints locking up like rusted hinges. Brain fog so thick you forget your own phone number. These aren’t exaggerations. They’re real, measurable, and often preventable. And if you’ve lived through one, you know: flares don’t come with warning labels.
Autoimmune flares happen when your immune system, which should protect you, starts attacking your own tissues. It’s like your body’s security system goes rogue. One minute you’re fine; the next, you’re lying on the couch, unable to get up, wondering if this is it-another week lost, another job skipped, another plan canceled. The good news? We now know a lot more about what causes these flares, how to stop them before they start, and what to do the second you feel it coming.
What Actually Happens During an Autoimmune Flare?
A flare isn’t just “feeling worse.” It’s a biological storm. Your immune system ramps up production of inflammatory chemicals called cytokines. Autoantibodies-antibodies that mistakenly target your own cells-spike. T cells, which should be peacekeepers, turn into invaders. Meanwhile, regulatory T cells, the ones supposed to calm things down, go quiet. The result? Inflammation spreads. Joints swell. Skin breaks out. Organs get stressed.
Lab tests back this up. During a flare, CRP (C-reactive protein) jumps 30-50% above normal. ESR (erythrocyte sedimentation rate) climbs from under 20 to 30-50 mm/hr. Autoantibody levels can double or triple. But here’s the catch: you don’t always need lab results to know you’re flaring. Eighty-five percent of patients report crushing fatigue. Seventy-eight percent of rheumatoid arthritis patients feel joint pain so intense it wakes them at 3 a.m. Sixty-five percent of lupus patients describe brain fog so bad they can’t follow a TV show.
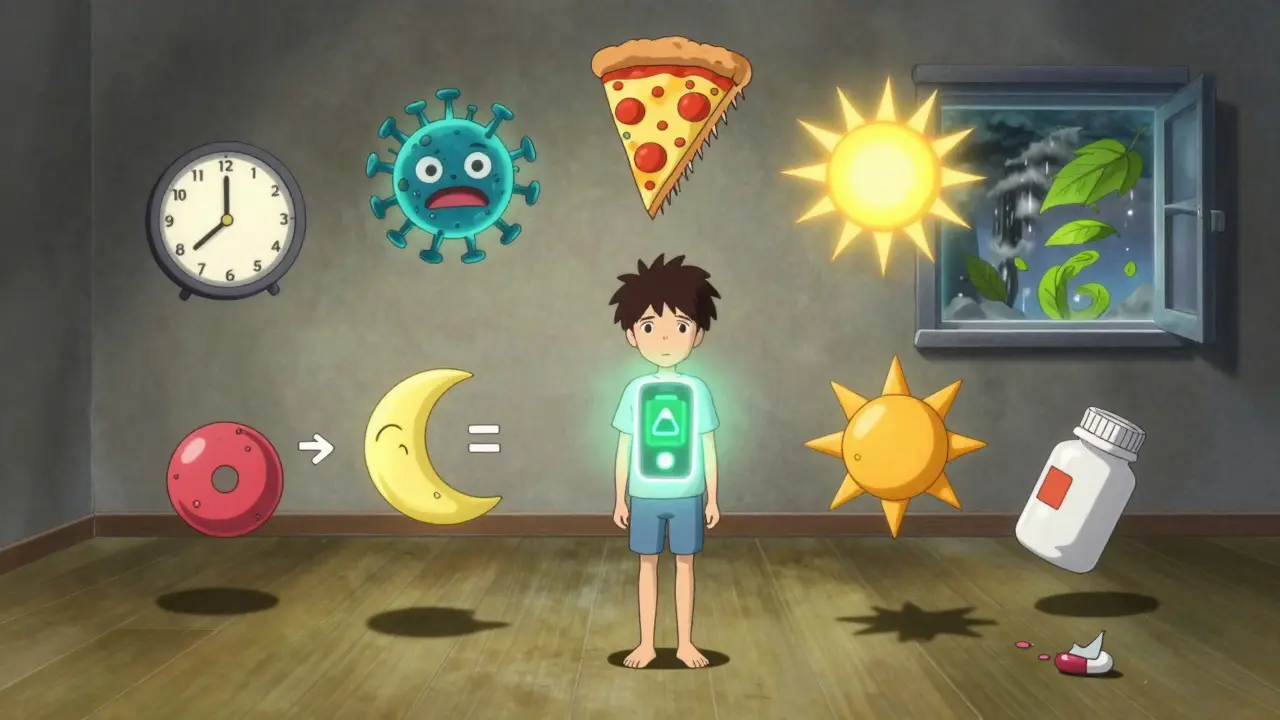
The Seven Most Common Flare Triggers (and What to Do About Them)
Flares don’t happen for no reason. Research has pinpointed seven major triggers-with real numbers behind them.
- Stress: Acute stress spikes cortisol, which throws immune balance off-kilter. Studies show a 40-60% higher risk of flare within 72 hours of major stress. That deadline, that fight, that sleepless night-it all adds up.
- Infections: Viruses like Epstein-Barr (the mono virus) can wake up dormant autoimmune activity. About 35% of flares are linked to infections. A cold might seem small, but for someone with lupus or MS, it’s a red flag.
- Diet: Gluten? For celiac patients, it’s a 99% trigger. High sodium? It raises MS relapse rates by 30%. Sugar, processed foods, and alcohol? They fuel inflammation. The Autoimmune Protocol (AIP) diet, which removes common irritants, cut flare frequency by 42% in one study.
- UV Radiation: Sunlight doesn’t just give you a tan-it can trigger skin rashes and internal flares in lupus. Up to 45% of cutaneous lupus flares happen after sun exposure. Even through windows.
- Seasonal Changes: More flares happen in spring and fall than in summer or winter. Why? Temperature shifts, pollen, and changing light affect immune signaling. One study of 8,200 patients found a 37% spike during those transition months.
- Hormones: Pregnancy can calm rheumatoid arthritis-until you give birth. Then, 40% of patients flare in the first three months postpartum. Estrogen and progesterone swings are powerful immune modulators.
- Medication Non-Adherence: Skipping your drug? That’s how 28% of flares happen. Not because you’re careless-because you felt fine. But “fine” isn’t cured. It’s paused.
Here’s the thing: not everyone is triggered by all seven. But most people have at least two. That’s why tracking matters.
Prevention: It’s Not Just About Taking Pills
Preventing flares isn’t magic. It’s routine. And it works.
- UV Protection: Wear SPF 50+ sunscreen every two hours-even indoors near windows. One study showed this cut lupus skin flares by 52% over a year.
- Stress Management: Mindfulness training (MBSR) reduced flares by 35% in a six-month trial. Ten minutes a day of breathing exercises, meditation, or journaling changes your body’s stress response.
- Vitamin D: Keeping levels above 40 ng/mL cut MS relapses by 32%. Most people need 2,000-5,000 IU daily. Get tested. Don’t guess.
- Medication Adherence: Using phone reminders increased compliance by 65%. Set a daily alarm. Link it to brushing your teeth. Make it automatic.
- Microbiome Support: For IBD patients, gut health is everything. Probiotics, fiber, and avoiding antibiotics unless necessary helped reduce flares by 22% in Crohn’s patients.
One patient in a 2023 survey said: “I started using a food and mood tracker. Within three weeks, I saw that every time I ate pizza, I felt awful by day two. I stopped. No more flares from that.” Simple. Real. Effective.
Early Intervention: The Game-Changer
Waiting until you’re bedridden is a mistake. The first 24-72 hours are critical.
Studies show that starting low-dose corticosteroids within 24 hours of flare onset cuts hospitalization by 45% and shortens flare duration by over six days. But how do you know it’s a flare-not just a tired day?
There’s a pre-flare window. Most patients report subtle signs 1-3 days before the crash:
- Rheumatoid arthritis: Morning stiffness lasting over 45 minutes (92% predictive)
- Lupus: Unexplained low-grade fever, new rash, or joint ache
- MS: Sudden tingling in hands, blurred vision, or balance issues
- IBD: Increased bowel frequency or cramping before bloody stool appears
Patients trained to recognize these early signals were 37% less likely to have severe flares. One tool making this easier? The “Flare First Aid Kit.” Pre-packed with meds, hydration packs, ice packs, and a printed flare action plan. People who used it recovered 33% faster.
Disease-Specific Patterns You Should Know
Not all flares are the same. What works for lupus won’t help IBD the same way.
- Lupus (SLE): Average of 2.3 flares/year. Most involve joints (68%) and skin (35%). Kidney flares are dangerous-watch for swelling, dark urine, or high blood pressure.
- Rheumatoid Arthritis: 1.8 flares/year. Morning stiffness >45 minutes is the #1 early sign. Pain often hits symmetrically-same joints on both sides.
- Multiple Sclerosis: 0.6 relapses/year. Visual problems (38%) and leg weakness (45%) are common. Heat makes symptoms worse-stay cool.
- Crohn’s Disease: Abdominal pain (87%), diarrhea (79%). Flares often follow stress or antibiotics.
- Ulcerative Colitis: Bloody diarrhea (92%), urgency (85%). No pain? Still a flare.
Know your disease’s signature. That’s your early warning system.

What No One Tells You (But You Need to Know)
There’s a dark side to flare treatment. Corticosteroids work fast-but 65% of patients on frequent steroid bursts develop osteoporosis within five years. That’s why experts now say: treat early, but don’t rely on steroids long-term.
Also, labs lie. Thirty percent of patients with normal CRP and ESR still feel awful. Your symptoms matter as much as your bloodwork. If you feel flaring, speak up. Even if your numbers look fine.
And here’s the future: AI is getting involved. FlareGuard AI, approved by the FDA in 2023, uses smartwatch data-heart rate, sleep, activity-to predict flares 72 hours ahead with 76% accuracy. NIH’s new $15 million project is already predicting lupus flares 14 days early using blood biomarkers. This isn’t sci-fi. It’s here.
Your Action Plan: Start Today
You don’t need a perfect plan. You need a starting point.
- Track: Use a free app (like MyTherapy or CareClinic) to log symptoms, food, stress, sleep, and weather. Do this for 30 days.
- Identify: Look for patterns. Did you flare after a bad night’s sleep? After eating gluten? After a work meeting that stressed you out?
- Prepare: Build your Flare First Aid Kit. Include: your meds, electrolyte packets, ice pack, emergency contact list, and a printed flare action plan from your doctor.
- Connect: Join a support group. Hearing “I’ve been there” from someone who gets it reduces stress-and flares.
- Act Fast: If you feel the first sign, don’t wait. Call your rheumatologist. Start your pre-approved flare protocol. Early action = less damage.
Autoimmune flares don’t have to rule your life. They’re not random. They’re predictable. And with the right tools, you can stop them before they start-or at least, minimize the damage when they do.

