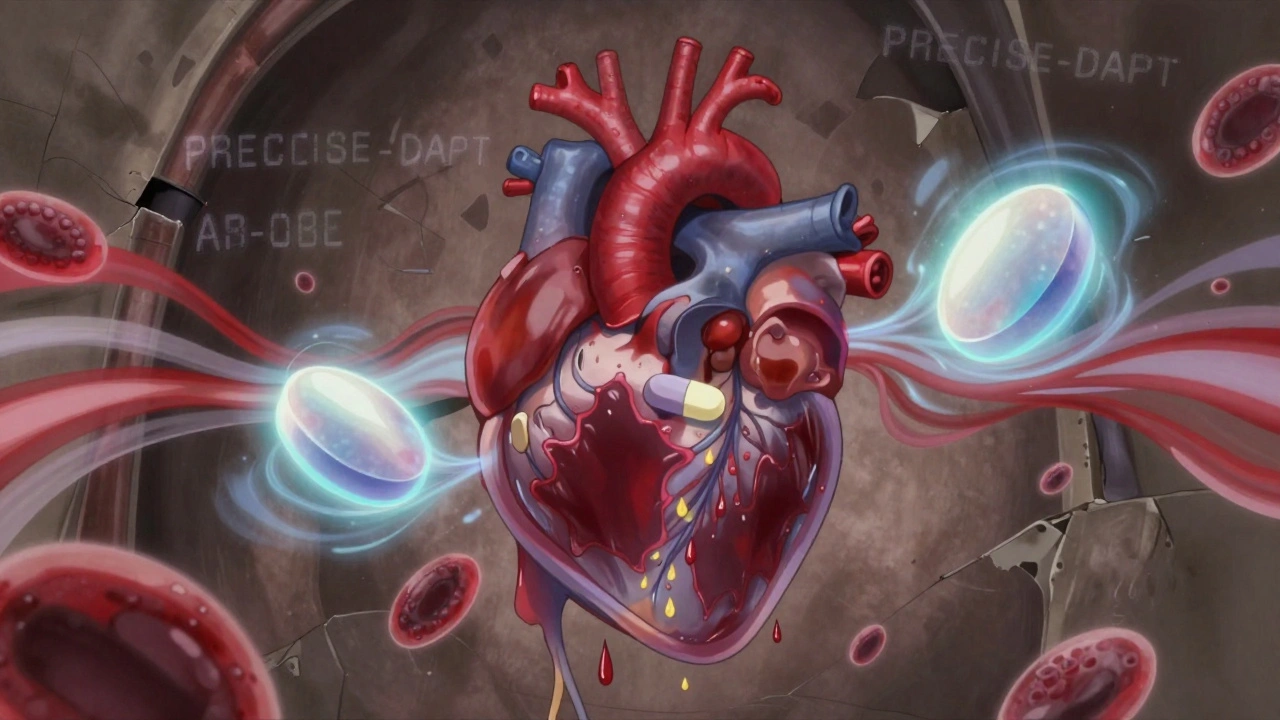
DAPT Bleeding Risk Calculator
Your Bleeding Risk Score
What Dual Antiplatelet Therapy Really Means for Your Body
Dual Antiplatelet Therapy, or DAPT, is a common treatment after a heart attack or stent placement. It combines two drugs-usually aspirin and a P2Y12 inhibitor like clopidogrel, prasugrel, or ticagrelor-to stop blood clots from forming in your arteries. This isn’t just a precaution. For many people, skipping DAPT means a high chance of another heart attack or stent failure. But there’s a trade-off: these same drugs make you bleed more easily.
Think of it like this: your blood needs to clot when you cut yourself, but it also needs to stay fluid inside your arteries. DAPT tips the balance toward fluidity to protect your heart. That’s why even a small cut can take longer to stop bleeding, or why you might notice nosebleeds or bruising more often. It’s not a flaw-it’s the intended effect. The problem comes when that effect goes too far.
The Real Bleeding Risks You Can’t Ignore
Major bleeding-like internal bleeding, heavy gastrointestinal bleeding, or bleeding that requires a hospital visit-happens in about 1-2% of patients on DAPT each year. That might sound low, but when you’re the one bleeding, it’s not. In the PLATO trial, patients on ticagrelor had a 27% higher risk of major bleeding than those on clopidogrel. And it’s not just about big events. Minor bleeding, called "nuisance bleeding," affects up to 15% of patients in the first month. That includes things like gum bleeding while brushing, frequent nosebleeds, or bleeding from minor scrapes that won’t stop after 10 minutes.
These small bleeds aren’t just annoying. They’re dangerous because they make people stop taking their meds. In the TALOS-AMI trial, patients with nuisance bleeding were 32% less likely to keep taking ticagrelor. And when people stop DAPT too early, their risk of stent clotting jumps 2-3 times. That’s why managing bleeding isn’t just about stopping the blood-it’s about keeping people alive by helping them stick with treatment.
Who’s at Highest Risk? The 6 Key Factors
Not everyone on DAPT has the same bleeding risk. Doctors now use tools like the PRECISE-DAPT score to figure out who’s most vulnerable. A score of 25 or higher means you’re in the high-bleeding-risk group. Here’s what pushes you into that category:
- Age 75 or older
- History of bleeding (even a simple nosebleed that needed packing)
- Low hemoglobin (below 10 g/dL) - a sign of anemia
- Chronic kidney disease (creatinine clearance under 60 mL/min)
- Low platelet count (under 100,000/μL)
- Taking blood thinners like warfarin or apixaban at the same time
If you fit even two of these, your doctor should be talking to you about shortening DAPT or switching to a safer combo. The 2021 consensus from the Academic Research Consortium says high-bleeding-risk patients have a 4% or higher chance of severe bleeding in a year. That’s not a small number. It’s a signal to adjust treatment.
Choosing the Right Drugs: Clopidogrel vs. Ticagrelor vs. Prasugrel
Not all DAPT regimens are created equal. The three P2Y12 inhibitors have different profiles:
| Drug | Dose | Strength of Platelet Inhibition | Major Bleeding Risk vs. Clopidogrel | Best For |
|---|---|---|---|---|
| Clopidogrel | 75 mg daily | Moderate | Baseline (lowest) | High bleeding risk, older adults |
| Prasugrel | 10 mg daily (5 mg if <60 kg or >75 yrs) | High | +30% higher | Diabetics, high clot risk |
| Ticagrelor | 90 mg twice daily | Very High | +27% higher | Patients under 75, no prior stroke |
Here’s the reality: ticagrelor and prasugrel are better at preventing heart attacks, but they cost you in bleeding. Clopidogrel is weaker at blocking clots but safer for your body. For someone over 75 with a history of stomach ulcers, clopidogrel might be the smarter pick-even if it’s not the strongest option. For a 52-year-old with diabetes and a recent heart attack, the extra protection from ticagrelor might be worth the risk.

Shortening DAPT: The New Standard for High-Risk Patients
For years, the rule was 12 months of DAPT after a stent. Now, we know that’s too long for many. The MASTER DAPT trial (2022) showed that for high-bleeding-risk patients, stopping DAPT after just one month and switching to aspirin alone cut major bleeding by 6.9% over two years-with no increase in heart attacks or death. That’s a game-changer.
Same with the Onyx ONE trial: 1-month DAPT followed by single therapy reduced bleeding by 5.3% without raising clot risk. These aren’t outliers. They’re the new baseline for care. If you’re high-risk, your doctor should be asking: "Do we really need 12 months?" Not "Do we need 6?"
De-escalation: Switching to a Safer Drug Mid-Treatment
Another smart move is de-escalation: starting with a strong drug like ticagrelor, then switching to clopidogrel after 1-3 months. The TALOS-AMI trial showed this cut major bleeding by 2.1% without increasing heart events. It’s like starting with a sledgehammer and then switching to a hammer-still effective, but less likely to break things.
This approach works best if you’re under 75, had a heart attack, and don’t have diabetes. It’s not for everyone, but for many, it’s the sweet spot between protection and safety. And it’s now endorsed by the FDA and EMA based on solid trial data.
What to Do If You Start Bleeding
If you notice blood in your stool, vomit that looks like coffee grounds, or a headache with sudden weakness-get help immediately. These aren’t normal side effects. They’re red flags.
For minor bleeding-like a nosebleed that lasts more than 10 minutes, or bleeding gums-you don’t need to panic. But you should call your doctor. Don’t stop your meds on your own. Instead, ask: "Should I switch to clopidogrel? Should we shorten the timeline?"
For procedures like dental work, colonoscopies, or even a simple biopsy, you usually don’t need to stop DAPT. The European Association of Percutaneous Cardiovascular Interventions says it’s safe for most minor procedures. The real danger is stopping and restarting. That’s when clots form.
Why Platelet Tests Don’t Help (And Might Hurt)
You might hear about platelet function tests-blood tests that measure how well your platelets are working. Some clinics offer them. Don’t fall for it.
The French Working Group on Perioperative Haemostasis says there’s no solid proof these tests improve outcomes. They’re expensive, inconsistent, and often lead to unnecessary changes in treatment. A 2022 study in the Journal of Thrombosis and Haemostasis found that patients who got these tests were more likely to have their meds changed, but their bleeding and clotting rates didn’t improve. Stick to clinical signs, not lab numbers.
Quality of Life: The Hidden Cost of Bleeding
Bleeding doesn’t just hurt-it changes how you live. In surveys, 68% of patients with minor bleeding reported anxiety about everyday activities. One woman stopped going to her book club because she was scared of bumping into someone and bleeding. Another man avoided shaving because his razor cuts wouldn’t stop. That’s not just physical-it’s emotional.
But here’s the good news: patients who switched to a safer DAPT plan reported a 15.3-point improvement in quality-of-life scores on the Seattle Angina Questionnaire. That’s a real difference. Less fear. More freedom. Better sleep. That’s what good care looks like.
The Future: Personalized DAPT Is Coming Fast
By 2028, 90% of heart patients will get DAPT tailored to their exact risk-not just their diagnosis. The DAPT-PLUS registry is tracking 15,000 people to build AI models that predict bleeding risk using age, kidney function, genetics, and even lifestyle. New reversal agents for ticagrelor and prasugrel are already in early trials. One, a P2Y12-Fc fusion protein, showed promise in animal studies at reversing platelet inhibition within minutes.
Right now, we’re stuck without a true antidote. Unlike warfarin (which can be reversed with vitamin K) or dabigatran (which has idarucizumab), we can’t just flip a switch to stop bleeding from DAPT. That’s why prevention and personalization matter more than ever.
What You Should Ask Your Doctor
If you’re on DAPT, here are five questions to ask at your next visit:
- What’s my PRECISE-DAPT score? Am I high-risk?
- Is my current P2Y12 drug the safest option for me?
- Can we shorten DAPT to 3 or 6 months instead of 12?
- Would switching to clopidogrel after a month reduce my bleeding risk?
- What signs of bleeding should I never ignore?
Don’t wait for bleeding to happen. Talk now. Your heart needs protection. But so does your body.
What Happens If You Stop DAPT Too Soon?
Stopping DAPT before 6 months-especially after a stent-doubles or triples your risk of stent thrombosis. That’s when a clot forms inside the stent and blocks blood flow. It’s a heart attack waiting to happen. The PARIS registry found that 70% of stent clots happened in patients who quit DAPT early, often because they were scared of bleeding.
But here’s the twist: stopping DAPT because your doctor told you to? That’s safe. The DAPT Study showed that when doctors guide the stop, even high-risk patients don’t have more heart events. It’s not about stopping. It’s about stopping the right way, at the right time, with the right plan.