Imagine dating someone who constantly battles secret urges to binge and purge. The dinner table becomes a battlefield, every compliment feels like a trigger, and intimacy can feel unsafe. That’s the hidden reality for many living with bulimia nervosa and the people they love. In this guide we’ll break down how the disorder reshapes emotions, communication, and trust across romantic, family, and friendship circles - and give you practical steps to support healing.
Understanding Bulimia Nervosa
Bulimia nervosa is a serious eating disorder characterized by recurrent binge‑eating episodes followed by compensatory behaviors such as self‑induced vomiting, laxative misuse, or excessive exercise. According to the National Eating Disorders Association, about 1.5% of women and 0.5% of men in the U.S. will experience bulimia at some point, and the average age of onset is 18‑24 years. The disorder isn’t just about food; it’s a coping mechanism for overwhelming emotions, often rooted in perfectionism, low self‑worth, and a need for control.
How Bulimia Affects Emotional Health
Beyond the physical toll, bulimia rewires the brain’s emotional circuitry. Chronic binge‑purge cycles trigger the release of stress hormones like cortisol, which amplifies feelings of Anxiety and Depression. The shame that follows a binge can spiral into a self‑critical loop, eroding Self‑esteem and fostering a sense of isolation. These emotional wounds don’t stay hidden; they spill into every interaction, coloring how a person perceives support, criticism, and love.
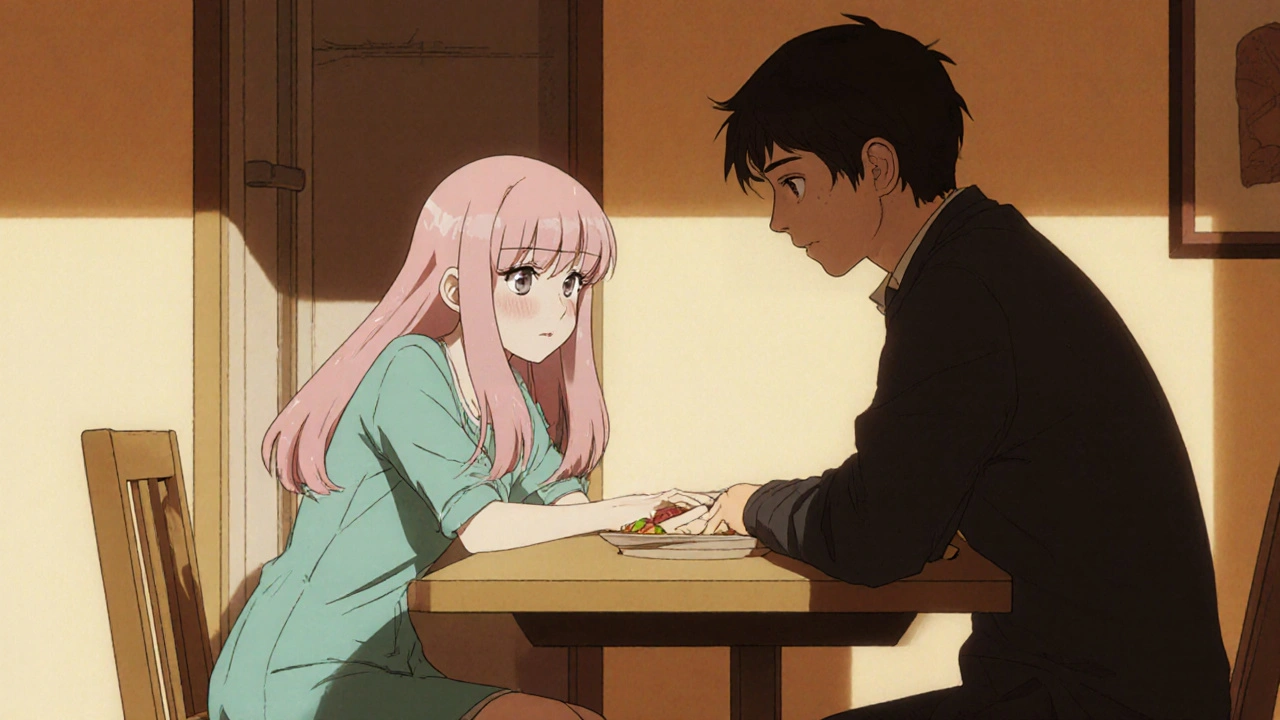
Impact on Romantic Partnerships
Intimate relationships are often the first to feel the strain. Trust becomes fragile when a partner discovers hidden eating behaviors or secret bathroom trips after meals. The secrecy breeds suspicion; even innocent inquiries can be interpreted as accusations, leading to defensive shutdowns. Sexual intimacy is also affected - many with bulimia report feeling uncomfortable with bodily exposure, pain during intercourse, or reduced libido due to hormonal imbalances. Over time, the couple may develop a pattern of conflict‑avoidance, where discussions about the disorder are postponed, creating emotional distance.
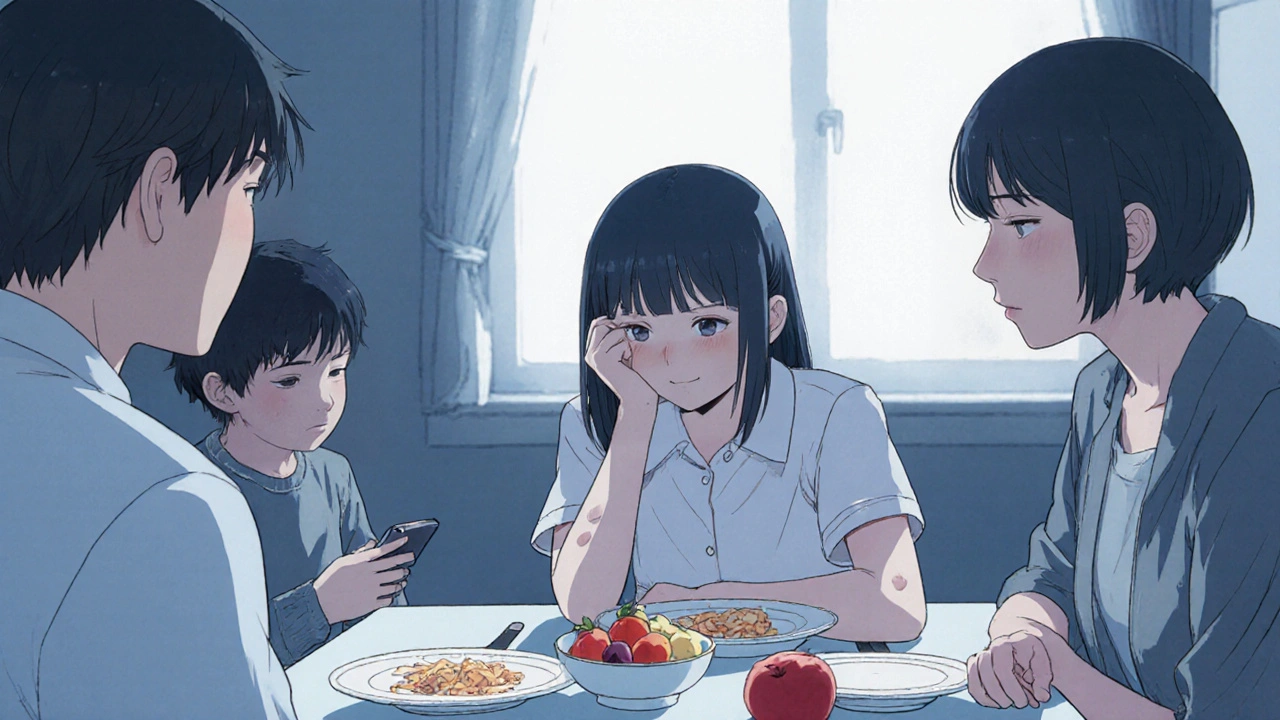
Family Dynamics and Bulimia
Families frequently oscillate between guilt and frustration. Parents might blame themselves for “causing” the disorder or, conversely, push for strict control over eating, which can intensify the binge‑purge cycle. Siblings may feel neglected as attention shifts to the affected member, breeding resentment. Family dynamics that emphasize perfection, criticism, or lack of emotional safety are common triggers. When families open up to honest conversation and seek professional guidance, they become a powerful source of recovery.
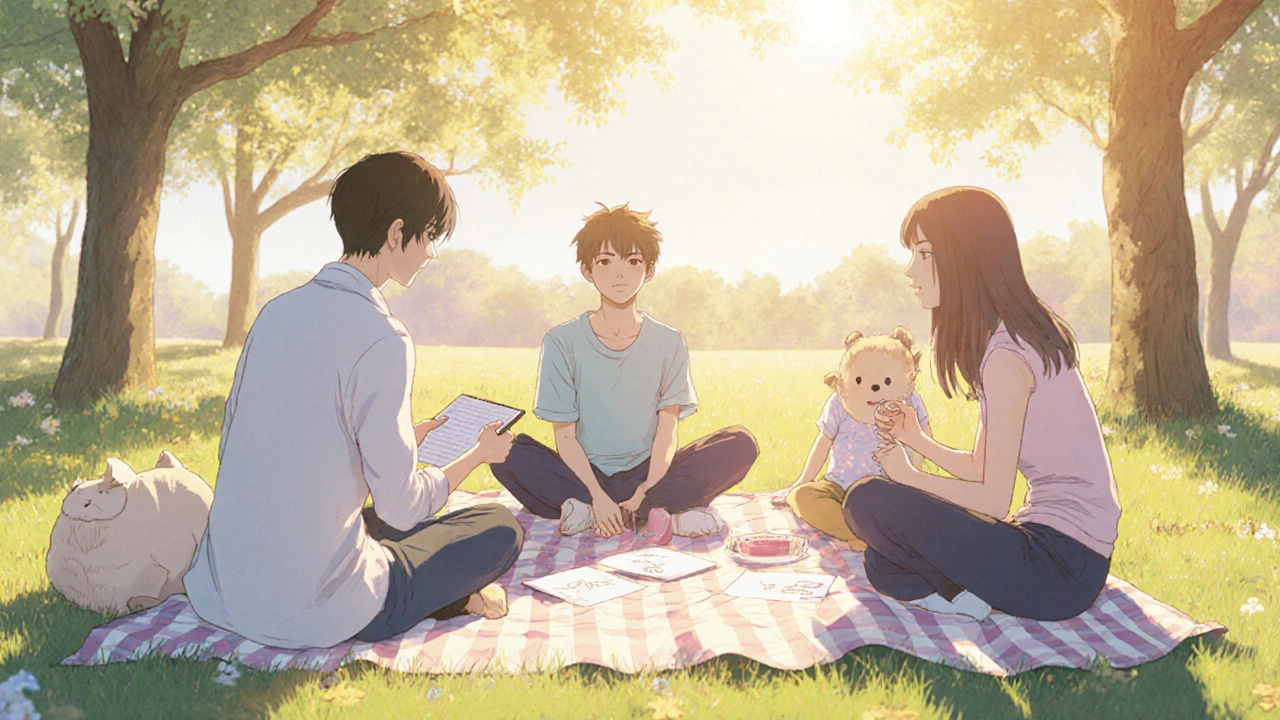
Friendships and Social Life
Outside the home, social stigma looms large. Friends might not understand why someone repeatedly “skips” meals or avoids group outings centered around food. The fear of judgment often leads to withdrawal, intensifying the sense of loneliness. Moreover, the disorder can cause mood swings that strain friendships - a sudden outburst of anger or a period of flat affect may be misread as disinterest. Maintaining friendships, therefore, requires patience, education, and clear boundaries.
Recognizing Red Flags in Relationships
Spotting the early signs can prevent deeper emotional damage. Look for these behaviors:
- Frequent trips to the bathroom after meals.
- Obsession with calories, weight, or body shape.
- Sudden avoidance of social eating events.
- Visible signs of enamel erosion, swollen cheeks, or calloused knuckles.
- Emotional volatility that seems linked to food‑related topics.
When you notice a pattern, approach the conversation with empathy-avoid blame, focus on observations, and express willingness to support.
Strategies for Supporting a Loved One
Support isn’t about fixing the disorder; it’s about creating a safe emotional environment while encouraging professional help. Effective approaches include:
- Active listening: Let the person share without interruption. Reflect back feelings (“It sounds like you feel trapped by the binge‑purge cycle”).
- Normalize treatment: Frame therapy as a strength, not a weakness. Highlight that Recovery process often involves nutrition counseling, cognitive‑behavioral therapy, and sometimes medication.
- Set boundaries: Clearly state what you can and cannot handle (e.g., “I can listen, but I’m not a therapist”).
- Educate yourself: Learn about the physiological effects of bulimia, such as electrolyte imbalance, to reduce fear and misinformation.
- Encourage balanced activities: Suggest non‑food‑related hobbies that foster self‑worth, like art, sports, or volunteering.
Remember, Social stigma often discourages disclosure. By offering non‑judgmental acceptance, you help break down that barrier.
Impact Summary Table
| Domain | Typical Emotional Effect | Common Behavioral Signs | Support Tips |
|---|---|---|---|
| Romantic | Trust anxiety, shame | Secret bathroom trips, avoidance of intimacy | Open dialogue, couple therapy, reinforce non‑food intimacy |
| Family | Guilt, conflict | Power struggles over meals, over‑monitoring | Family counseling, shared meals without pressure |
| Friendship | Isolation, fear of judgment | Skipping gatherings, mood swings | Invite to non‑food activities, educate peers |
| Self‑Concept | Low self‑esteem, self‑criticism | Negative self‑talk, body checking | Positive affirmation, CBT techniques |
Moving Forward - Hope and Healing
Recovery is rarely a straight line; setbacks happen, but each step toward openness builds resilience. When a loved one begins therapy, celebrate the courage rather than the speed of progress. Encourage them to track emotions, not just calories, because identifying triggers is the first move toward breaking the binge‑purge loop. Over time, healthier communication patterns replace secrecy, and relationships can evolve into sources of strength rather than stress.
Frequently Asked Questions
Can bulimia nervosa develop in a relationship that seems stable?
Yes. Even in loving, supportive partnerships, the pressures of perfectionism, body image, or stress can spark binge‑purge behaviors. A stable relationship may mask symptoms until they become severe.
How can I talk to my partner about suspected bulimia without causing defensiveness?
Choose a calm moment, use “I” statements, and focus on observed behaviors, not judgments. Example: “I’ve noticed you often go to the bathroom after dinner and I’m worried about you. I’m here if you want to talk.”
What role does anxiety play in the binge‑purge cycle?
Anxiety often triggers a binge as a coping mechanism, followed by purging to regain a sense of control. The cycle reinforces the brain’s reward pathways, making it harder to break without addressing the underlying anxiety.
Is it possible for a family member to unintentionally worsen bulimia?
Yes. Over‑monitoring meals, commenting on weight, or imposing strict diets can heighten the person’s sense of pressure, leading to more secretive behaviors. Compassionate, non‑judgmental support works better.
What professional resources are most effective for bulimia recovery?
Cognitive‑behavioral therapy (CBT‑E) is the gold standard, often combined with nutrition counseling and, when needed, antidepressant medication. Multi‑disciplinary care that includes medical monitoring is crucial.