When you pick up a generic pill, you assume it’s the same as the brand-name version. Same active ingredient. Same effect. Same price. But what if the problem isn’t the drug itself - but what’s hiding in the filler?
What Exactly Are Excipients?
Excipients are the non-active parts of a pill. They don’t treat your condition. They don’t fight infection or lower blood pressure. But they do hold the medicine together, help it dissolve, make it taste better, or keep it from going bad. Common ones include lactose (a milk sugar), cornstarch, magnesium stearate, FD&C dyes, and preservatives like parabens. The FDA calls them "inactive" - but that’s misleading. In 2019, a study of over 42,000 oral medications found that 90.2% of them contained at least one ingredient known to cause allergic reactions or intolerance in sensitive people. The average pill had 8.8 excipients. Some of the most prescribed drugs had more than 80 different inactive ingredient combinations across different brands.Why Does This Matter?
You might think: "I’m lactose intolerant. I’ll just avoid dairy." But lactose is in 40-60% of all oral tablets. A single pill can contain 50-200 milligrams of it. For someone with mild intolerance, that’s enough to trigger bloating, cramps, or diarrhea. And you won’t know it’s the pill unless you connect the dots. Same with artificial colors. Yellow #5 and Blue #2 are used to make pills look different - not for function, but for branding. People with sensitivities report hives, headaches, or stomach pain after switching to a generic version that suddenly includes these dyes. One Reddit user switched from brand-name Synthroid to a generic and developed severe GI distress. Turns out, the generic had FD&C Blue #2 - something the brand version never contained.Generics Aren’t Always Identical
The FDA requires generics to be bioequivalent - meaning they deliver the same amount of active drug into your bloodstream as the brand. But that’s it. They don’t have to match the excipients. A 2021 study found that 73.5% of pharmacists had patients complain about differences in how they felt after switching from brand to generic. Symptoms? Nausea, headaches, fatigue, diarrhea - things that weren’t there before. These aren’t side effects of the drug. They’re reactions to the filler. Even two different generics of the same drug can have different excipients. One manufacturer might use lactose. Another might use mannitol. One might use talc. Another might use cellulose. The active ingredient is the same. But your body might react differently.
Who’s Most at Risk?
Not everyone will notice. But certain groups are more vulnerable:- Lactose-intolerant people: As little as 1-2 grams of lactose can trigger symptoms in sensitive individuals. A single tablet might contain 100-200 mg. That’s not a lot - but if you’re taking five pills a day, you’re hitting 1 gram. Add in yogurt, cheese, or bread with lactose, and you’re over the limit.
- People with celiac disease: Some generics use wheat starch as a filler. Even trace amounts can cause damage.
- Those with allergies to dyes: Red #40, Yellow #5, Blue #1 - these are common in pediatric and branded generics. Reactions range from skin rashes to behavioral changes in kids.
- People on multiple medications: If you’re on five or more pills a day, you’re exposed to dozens of excipients. Cumulative exposure matters.
- Children and elderly patients: Their bodies process fillers differently. Their tolerance thresholds are lower.
What to Do If You Suspect an Excipient Reaction
If you start feeling worse after switching to a generic - especially if it’s a new symptom - don’t assume it’s "just in your head." Here’s what to do:- Track your symptoms. Write down when they started, how often they happen, and what pills you took that day.
- Check the ingredient list. Look up the generic version on the FDA’s Inactive Ingredient Database or Pillbox (run by the National Library of Medicine). Compare it to the brand you were on.
- Ask your pharmacist. Pharmacists have access to manufacturer sheets. They can tell you exactly what’s in each version. Most won’t bring it up unless you ask.
- Try switching back. If symptoms disappear when you go back to the original version, you’ve found your trigger.
- Document it. Tell your doctor. Ask them to note "excipient intolerance" in your chart. This helps avoid future switches.
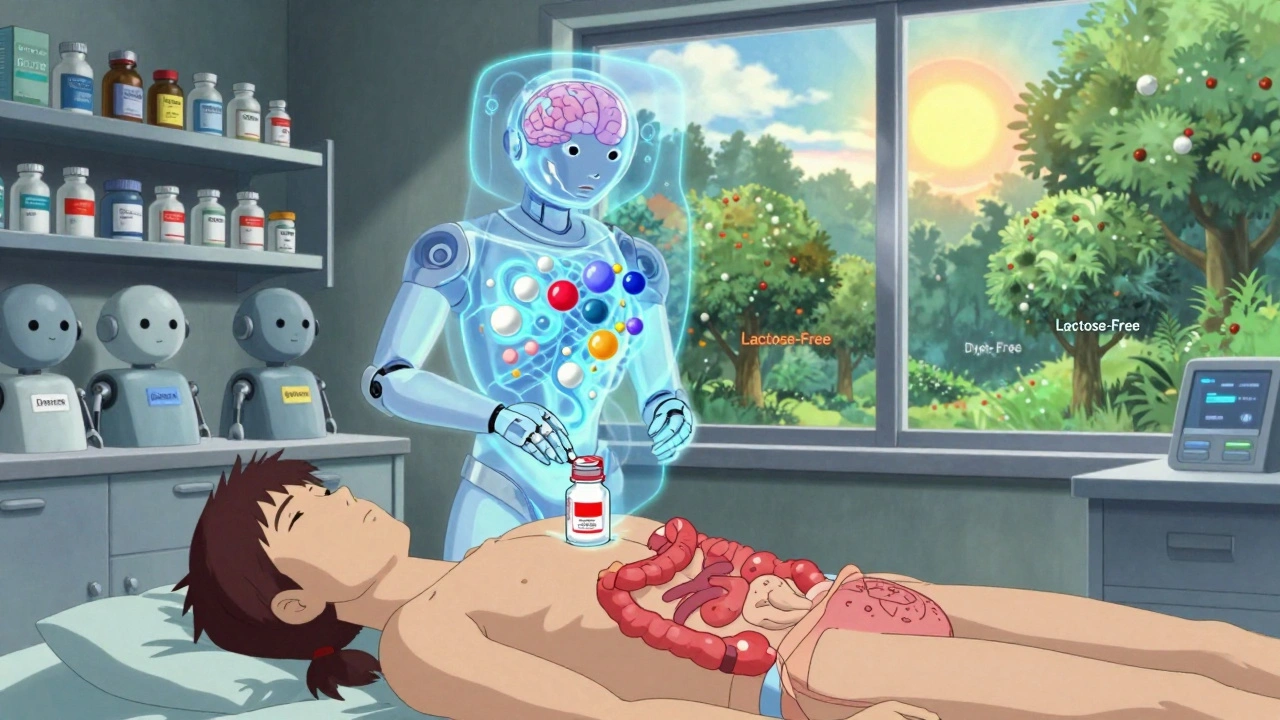
How to Find Safer Generics
You don’t have to stick with expensive brands. But you do need to be smarter about choosing generics.- Look for "lactose-free," "dye-free," or "gluten-free" labeled generics. These are becoming more common.
- Ask your pharmacist to source a generic from a manufacturer known for cleaner formulations. Some companies specialize in low-excipient products.
- Use resources like the Inactive Ingredients Book by Raymond C. Rowe - it’s the industry bible for excipient safety.
- Check if your insurance allows brand-name exceptions for documented excipient intolerance. Many do.
The Bigger Picture
The generic drug market is huge - over 90% of U.S. prescriptions are filled with generics. That’s good for costs. But it’s bad for safety if we ignore what’s inside. The FDA is starting to catch on. In 2023, they launched the Excipient Safety Modernization Initiative, which will start including patient-reported reactions in their databases. MIT is developing an AI tool that predicts your personal tolerance based on genetics. By 2025, the FDA plans to require full excipient disclosure in electronic prescriptions. Meanwhile, the market for specialty excipients - lactose-free, dye-free, hypoallergenic - is growing fast. It hit $18.7 billion in 2022 and is rising at nearly 7% a year. That tells you something: patients are speaking up. And companies are listening.Final Thought: "Inactive" Doesn’t Mean Harmless
Just because an ingredient doesn’t treat your condition doesn’t mean it’s harmless. Excipients are the silent players in your medication. They’re not just fillers. They’re triggers. They’re barriers to adherence. They’re why some people stop taking their meds - not because the drug doesn’t work, but because it makes them feel worse. Your health isn’t just about the active ingredient. It’s about the whole pill. And if you’re sensitive, you deserve to know what’s in it.Can excipients in generics cause real side effects?
Yes. While excipients don’t treat disease, they can cause allergic reactions, digestive issues, headaches, or skin rashes in sensitive individuals. Common culprits include lactose, artificial dyes (like Yellow #5 and Blue #2), parabens, and gluten-containing fillers. A 2019 study found 90.2% of oral medications contain at least one ingredient linked to adverse reactions.
Are all generic drugs the same in terms of ingredients?
No. While generics must match the active ingredient and bioavailability of the brand, they can use completely different excipients. Two different manufacturers’ versions of the same generic drug may contain different fillers, binders, or dyes. This is why some people tolerate one generic but react to another.
How can I find out what excipients are in my generic medication?
Check the FDA’s Inactive Ingredient Database (IID) or use Pillbox, a free tool from the National Library of Medicine. You can also ask your pharmacist for the manufacturer’s ingredient list - they have access to it. Brand-name drugs usually list everything on the packaging; generics often require a direct request.
Is lactose really a problem in pills?
Yes. Lactose is used in 40-60% of oral tablets. For someone with lactose intolerance, even 1-2 grams per day can cause bloating, gas, or diarrhea. A single tablet may contain 100-200 mg. If you take five pills a day, you’re consuming up to 1 gram - enough to trigger symptoms in sensitive people.
Should I avoid generics because of excipients?
No. Generics are safe and effective for most people. But if you have known allergies, intolerances, or unexplained symptoms after switching, investigate the excipients. Many manufacturers now offer lactose-free, dye-free, or gluten-free versions. Talk to your pharmacist - you can often find a compatible generic without paying brand prices.
What should I do if I think an excipient is making me sick?
Track your symptoms and match them to when you switched medications. Compare the ingredient lists of your old and new pills. Talk to your pharmacist and doctor. Ask to switch back to the version that worked, or request a different generic manufacturer. Document your reaction in your medical record - this prevents future switches that could trigger the same issue.
More people are starting to notice this. And as awareness grows, so will the options. Your body doesn’t care if a pill is cheap. It only cares what’s in it.

