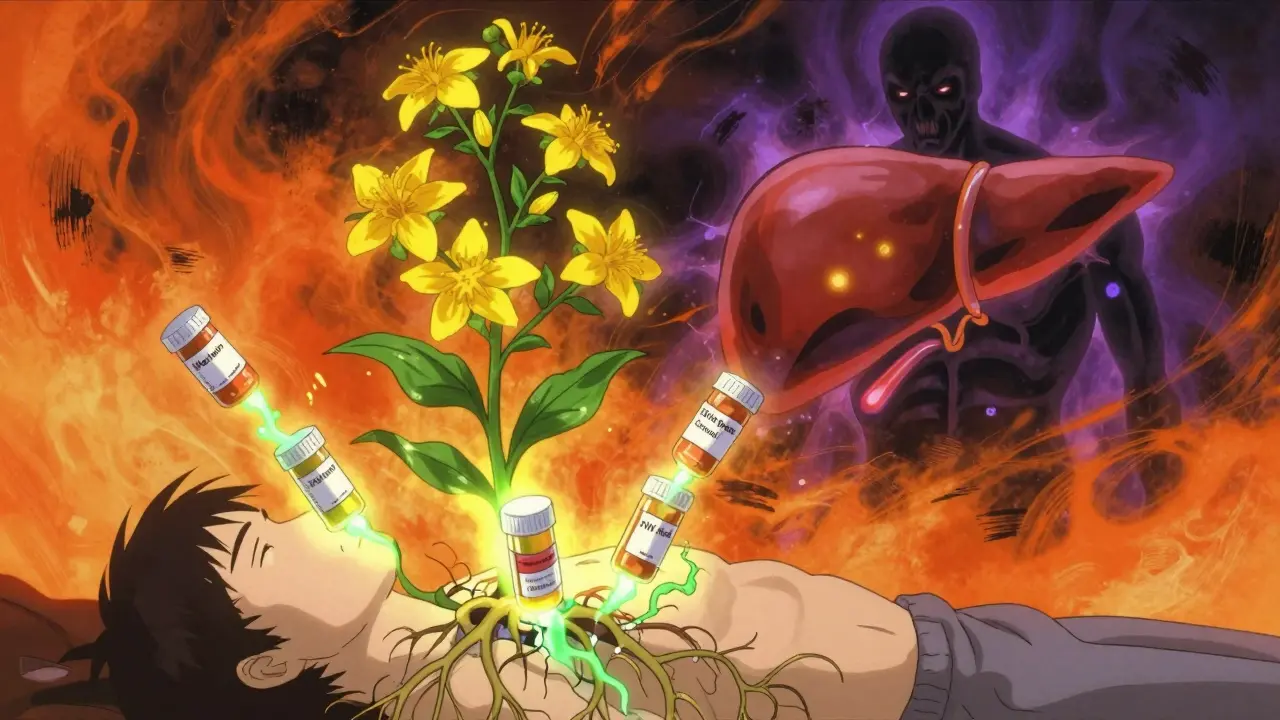
St. John’s Wort isn’t just another herbal pill on the shelf. For many, it’s a go-to for low mood, anxiety, or sleep troubles. But what most people don’t realize is that this plant, with its bright yellow flowers, can quietly undo the effects of life-saving medications. If you’re taking anything from birth control to HIV drugs to transplant meds, St. John’s Wort could be silently lowering their effectiveness - and putting your health at risk.
How St. John’s Wort Changes How Your Body Processes Drugs
St. John’s Wort works by turning up a key system in your liver called the cytochrome P450 enzyme, especially CYP3A4. Think of this enzyme as a factory worker that breaks down drugs so your body can get rid of them. When St. John’s Wort wakes up this factory, it starts working overtime. The active ingredient behind this is hyperforin, found in the plant’s flowers and leaves. Standard extracts with 3-5% hyperforin can double or even triple how fast your body clears out other medicines. This isn’t a slow effect - it kicks in within a week of starting the supplement and can last for two weeks after you stop taking it.
This isn’t theoretical. Studies show that when people take St. John’s Wort alongside certain drugs, those drugs vanish from their bloodstream much faster than they should. The result? The medication simply doesn’t work like it’s supposed to.
Warfarin and Blood Thinners: A Silent Danger
If you’re on warfarin (Coumadin) or phenprocoumon (Marcoumar), your blood clotting levels are carefully monitored with regular INR tests. These drugs keep you from having dangerous clots - but they’re a tightrope walk. Too little, and you risk a stroke or pulmonary embolism. Too much, and you could bleed internally.
St. John’s Wort throws that balance off. Between 1998 and 2000, European health agencies recorded 22 cases where people on stable warfarin doses suddenly saw their INR drop by 50% or more after starting St. John’s Wort. One 62-year-old man’s INR fell from 2.8 to 1.4 in just seven days. That’s not just a number - it’s a ticking time bomb. The same thing happens with phenprocoumon. A 2006 study found that 12 patients taking 900 mg of St. John’s Wort daily had a 37% drop in their phenprocoumon levels. No warning. No symptoms. Just a silent failure of your blood thinner.
Transplant Patients: A Life-Threatening Risk
For someone who’s had a kidney, liver, or heart transplant, immunosuppressants like cyclosporine and tacrolimus aren’t optional - they’re survival tools. These drugs keep your immune system from attacking your new organ. But St. John’s Wort doesn’t care. It speeds up their breakdown.
A 2004 study of 10 kidney transplant patients found that adding St. John’s Wort caused cyclosporine levels to crash by 54%. Two of those patients had acute transplant rejection. Tacrolimus isn’t any safer - one study showed levels dropping by up to 60%. The European Medicines Agency issued a formal warning in 2007 after reviewing 17 cases of transplant rejection tied to this interaction. If you’ve had an organ transplant, taking St. John’s Wort isn’t a risk - it’s a gamble with your life.
Birth Control: The Hidden Pregnancy Risk
Many women assume herbal supplements are safe alongside birth control. They’re wrong. St. John’s Wort reduces the levels of both estrogen and progestin in oral contraceptives. A 2005 study found that women taking a common St. John’s Wort extract had a 15.4% drop in estrogen and a 25.6% drop in progestin. That’s enough to make birth control fail.
The Swedish Medical Products Agency documented 47 cases of contraceptive failure between 2000 and 2003 - 12 of them resulted in confirmed pregnancies. GoodRx’s 2022 analysis of FDA reports found 217 cases where women got pregnant while taking St. John’s Wort and birth control together. And here’s the kicker: a 2023 Consumer Reports survey showed only 32% of supplement users knew this was even a possibility. If you’re on the pill, patch, or ring - skip St. John’s Wort entirely.

HIV Medications: A Recipe for Drug Resistance
For people living with HIV, missing even a single dose of antiretroviral drugs can lead to resistance. St. John’s Wort doesn’t just miss doses - it makes them useless. A 2004 study in Clinical Infectious Diseases showed that St. John’s Wort cut the blood levels of indinavir, a key HIV protease inhibitor, by 57% on average. Some individuals saw reductions as high as 99%.
One UK patient saw their viral load spike after starting St. John’s Wort while on indinavir and lamivudine. The virus rebounded. Drug resistance followed. The U.S. Department of Health and Human Services explicitly warns against using St. John’s Wort with any protease inhibitor or certain non-nucleoside reverse transcriptase inhibitors. There is no safe level of this interaction.
Serotonin Syndrome: When Mood Boosters Turn Deadly
St. John’s Wort boosts serotonin - that’s why it helps with mild depression. But if you’re already taking an SSRI like fluoxetine (Prozac), an SNRI like venlafaxine (Effexor), or even 5-HTP or melatonin, you’re stacking serotonin on top of serotonin. That’s how serotonin syndrome starts.
Symptoms include abnormal sweating (89% of cases), heart rate over 100 bpm (76% of cases), muscle spasms (63% of cases), and confusion (92% of cases). In 2021, an 18-year-old man in New Zealand was rushed to the hospital after taking St. John’s Wort with 5-HTP and Adderall. He had a heart rate of 128 bpm, high blood pressure, and bizarre paranoid behavior. He needed IV fluids and benzodiazepines to calm his nervous system. This isn’t rare. Poison Control centers see these cases every year.
Other Dangerous Interactions You Can’t Ignore
St. John’s Wort doesn’t stop at antidepressants and birth control. It messes with:
- Benzodiazepines like Xanax - reduces effectiveness by up to 40%, leaving anxiety uncontrolled.
- Digoxin (Lanoxin) - lowers blood levels by 25%, risking heart failure.
- Phenytoin (Dilantin) - cuts levels by 19-46%, increasing seizure risk. The FDA received 12 reports of breakthrough seizures between 2000-2005.
- Alprazolam - same story. Less drug in your blood means less relief.
Each of these interactions has been confirmed in multiple clinical studies. This isn’t speculation. It’s documented risk.
What Experts Are Saying - And What You Should Do
Dr. Paul Farmer from the National Center for Complementary and Integrative Health called St. John’s Wort “one of the highest risk herbal supplements for clinically significant drug interactions.” The European Medicines Agency now requires every product to carry a bold warning about 17 medication classes. The FDA is taking steps too - by January 2025, all St. John’s Wort labels in the U.S. must include a “Drug Interaction Alert” symbol.
Here’s what you need to do:
- If you’re on any prescription medication - especially blood thinners, birth control, HIV drugs, or immunosuppressants - don’t take St. John’s Wort.
- If you’re already taking it, tell your doctor or pharmacist. Don’t quit cold turkey - stopping suddenly can cause withdrawal symptoms.
- Ask your pharmacist to run your meds through the St. John’s Wort Drug Interaction Checker. It lists 142 known interactions.
- If you’re switching from an SSRI to St. John’s Wort, wait at least 14 days between stopping the drug and starting the herb. The American Psychiatric Association recommends this to avoid serotonin syndrome.
And here’s the hard truth: even if you’re healthy, you might not know what’s in your supplement. A 2023 Consumer Reports survey found that 82% of users didn’t know about the birth control risk. Only 18% knew about the HIV interaction. Labels are often vague. The supplement industry isn’t held to the same standards as pharmaceuticals. You can’t assume safety.
The Future: Can We Make It Safer?
Researchers are working on it. A 2023 clinical trial tested a new type of St. John’s Wort extract with hyperforin levels below 0.5%. The results? It worked just as well for depression - but caused only a 9% drop in a key liver enzyme marker, compared to 56% with standard extracts. This suggests it might be possible to keep the mood benefits without the dangerous interactions.
The National Institutes of Health is funding a $2.4 million study to explore this further, with results expected by late 2024. Until then, stick to the facts: if you’re on medication, St. John’s Wort isn’t worth the risk.
Can I take St. John’s Wort if I’m not on any medication?
Even if you’re not on prescription drugs, St. John’s Wort can still cause side effects like dry mouth, dizziness, or increased sun sensitivity. It’s not a harmless herb. And if you start taking medications later - even something as simple as an antibiotic or ibuprofen - the interaction risk kicks in. It’s safer to avoid it unless you’re under medical supervision.
Is St. John’s Wort regulated like a drug?
No. In the U.S. and many other countries, it’s sold as a dietary supplement, which means manufacturers don’t need to prove safety or effectiveness before selling it. The FDA can only act after harm is reported. That’s why 17 warning letters were issued to manufacturers between 2019 and 2023 - for failing to warn about drug interactions. You can’t trust the label alone.
How long does it take for St. John’s Wort to start interacting with drugs?
The enzyme-inducing effect can begin within 7-14 days of starting the supplement. It’s not immediate, which is why many people don’t connect the dots. If you started taking St. John’s Wort two weeks ago and your blood pressure or mood suddenly changed, it could be the supplement.
Can I take St. John’s Wort with over-the-counter painkillers like ibuprofen or acetaminophen?
There’s no strong evidence of serious interaction with ibuprofen or acetaminophen. But since St. John’s Wort affects liver enzymes, it’s still possible to alter how your body processes these drugs over time. If you’re taking them regularly, it’s best to talk to your pharmacist. Better safe than sorry.
What should I do if I’ve already taken St. John’s Wort with my medication?
Don’t panic, but don’t ignore it either. Stop taking St. John’s Wort immediately and contact your doctor or pharmacist. If you’re on warfarin, HIV meds, or immunosuppressants, you may need urgent blood tests to check drug levels. For birth control, use backup contraception for at least 2 weeks after stopping. If you feel unwell - racing heart, confusion, seizures, or unusual bleeding - go to the emergency room.
Next Steps: Protecting Yourself
Before starting any new supplement, ask: “What else am I taking?” Write down every pill, patch, or drop you use - including vitamins, OTC meds, and herbal products. Bring that list to your next doctor or pharmacist visit. Don’t assume they’ll ask. Most don’t. And if someone tells you herbal means safe, they’re wrong. St. John’s Wort is one of the most dangerous supplements on the market - not because it’s toxic, but because it quietly breaks the rules your body uses to process life-saving drugs.