Before you write a prescription, you need to know if the drug your patient needs is covered-and at what cost. Skipping this step isn’t just a paperwork oversight; it’s a risk to their health and your practice’s efficiency. In 2025, nearly 70% of U.S. prescribers still waste 10-20 minutes per patient verifying coverage, often because they’re checking the wrong formulary version or missing a prior authorization requirement. That’s time that could be spent on care, not bureaucracy.
What Exactly Is a Formulary?
A formulary, also called a Preferred Drug List (PDL), is the official list of medications an insurance plan will pay for. It’s not random. Every drug on it has been reviewed by a committee of doctors and pharmacists who weigh clinical evidence, safety, and cost. These lists are updated regularly-sometimes monthly-to reflect new studies, FDA approvals, or pricing changes. Medicare Part D plans follow a strict five-tier system:- Tier 1: Preferred generics-often $1-$5 per prescription
- Tier 2: Non-preferred generics-usually $10-$20
- Tier 3: Preferred brand-name drugs-$40-$70
- Tier 4: Non-preferred brands-$80-$150+
- Tier 5: Specialty drugs-costs over $950/month, paid as a percentage (coinsurance)
Key Codes You Must Know
Every drug listing includes one or more codes that tell you what’s required before the pharmacy can fill it:- PA (Prior Authorization): The insurer needs documentation proving medical necessity before approving the drug.
- ST (Step Therapy): The patient must try and fail on a cheaper, preferred drug first.
- QL (Quantity Limit): Only a certain amount (e.g., 30 tablets) is covered per month.
How to Check a Formulary: Four Reliable Methods
You don’t need to memorize every plan’s list. Here’s how to check fast and accurately:- Use the insurer’s online drug search tool-Most major insurers (Aetna, UnitedHealthcare, Humana) have searchable databases. You’ll need the patient’s plan name and sometimes their zip code. Aetna’s tool, for example, shows tier level and PA requirements in real time. Providers rated it “very helpful” in 74% of cases.
- Check your EHR system-If your practice uses Epic, Cerner, or another major platform, they likely have a built-in formulary checker. Northwestern Medicine cut prescription abandonment by 42% after enabling Epic’s Formulary Check module in 2023.
- Call the plan’s provider hotline-98% of Medicare Part D plans offer 24/7 provider lines. If you’re unsure about a drug’s status or need help with a prior auth, this is faster than waiting for an email reply.
- Use CMS Plan Finder-For Medicare patients, this free tool covers 99.8% of Part D plans. You can search by drug name, see tier placement, and check for restrictions. It’s updated monthly.
Differences Between Medicare, Medicaid, and Commercial Plans
Don’t assume all formularies work the same. Here’s how they differ:| Feature | Medicare Part D | Medicaid | Commercial (e.g., UnitedHealthcare) |
|---|---|---|---|
| Tier Structure | 5 tiers (standardized) | Usually 3-4 tiers, often closed | 4 tiers common, varies by plan |
| Formulary Type | Open (exceptions required) | Closed (prior auth for non-listed drugs) | Mostly open |
| Update Frequency | Quarterly with 60-day notice | Varies by state, often annual | Monthly or quarterly |
| Specialty Drug Access | Tier 5, coinsurance-based | Often requires PA + prior treatment failure | May require specialty pharmacy |
| Expedited PA Response Time | 24 hours for urgent cases | Varies by state | Usually 72 hours |
What’s Changing in 2025
New rules are reshaping how formularies work:- $2,000 out-of-pocket cap for Medicare Part D starts January 2025. Plans are shifting more drugs to lower tiers to help patients hit the cap faster.
- Real-time benefit tools (RTBT) will be mandatory for all Medicare Part D plans by January 2026. This means formulary and cost data will auto-populate in your EHR when you type in a drug name.
- AI tools like Epic’s FormularyAI now predict coverage likelihood with 87% accuracy by analyzing past prior auth decisions.
Common Mistakes and How to Avoid Them
Here’s what goes wrong-and how to fix it:- Mistake: Assuming all Medicare plans are the same. Fix: Always verify by patient-specific plan ID, not just “Medicare Part D.”
- Mistake: Using last year’s formulary. Fix: Bookmark the insurer’s formulary page and set quarterly calendar reminders. HealthPartners, for example, updates in January, April, July, and October.
- Mistake: Prescribing a Tier 4 drug without checking alternatives. Fix: Ask yourself: “Is there a Tier 1 or Tier 3 equivalent?” Generic metformin is often just as effective as a branded version.
- Mistake: Not documenting prior auth attempts. Fix: Log every request in the patient’s chart-date, time, outcome. It helps if they need to appeal later.
Pro Tips for Busy Clinics
- Start with the patient’s plan card. The plan name is printed right on it. Use that to search. - Keep a printed cheat sheet for your top 10 prescribed drugs across your most common plans. Update it every quarter. - Train your staff. Have a medical assistant run the formulary check before the patient even sees you. Saves 15 minutes per visit. - Use templates. In your EHR, create a formulary check note template: “Drug: ___, Tier: ___, PA: Yes/No, ST: Yes/No, QL: ___.”When Formularies Hurt Care
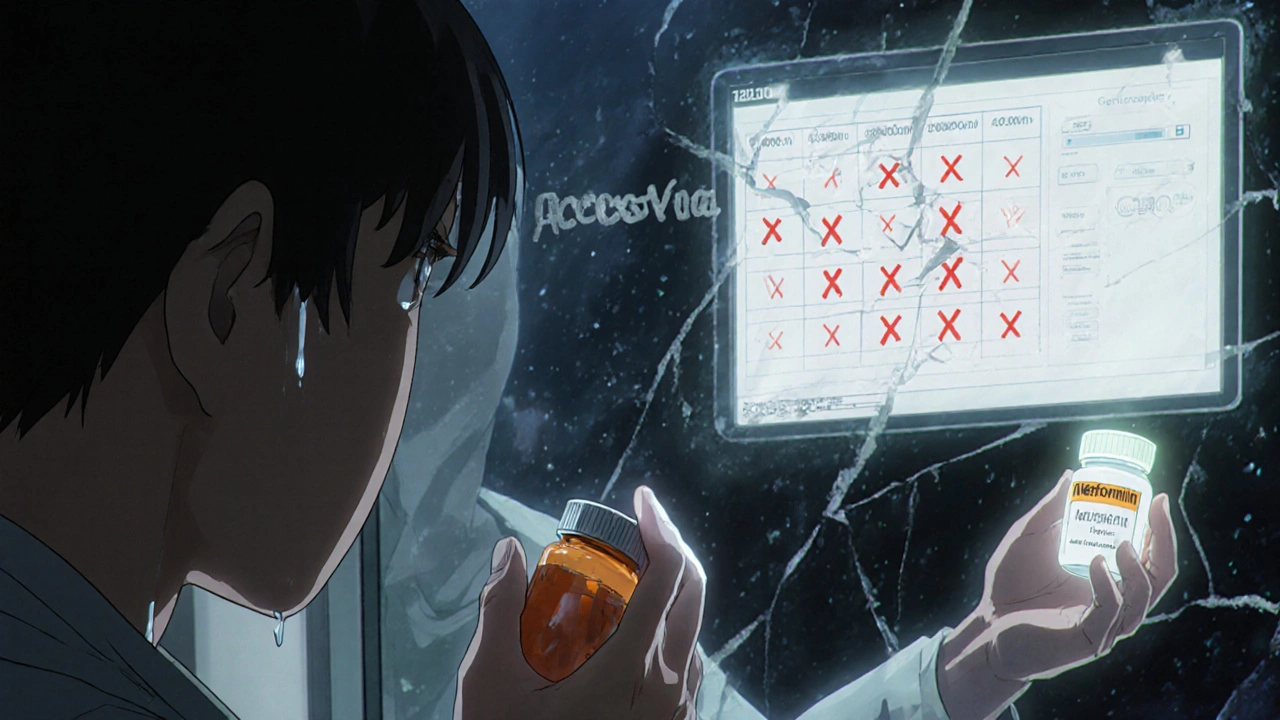
Formularies are meant to save money and improve outcomes. But sometimes, they don’t. Dr. Aaron Kesselheim from Brigham and Women’s Hospital found that 32% of prior auth requests for cancer drugs take over 48 hours to process. That’s not just a delay-it’s a threat to survival. And it’s not just cancer. Patients with diabetes, depression, or autoimmune diseases often face the same barriers. When a patient can’t get their drug on time, they skip doses. Or worse-they don’t fill the prescription at all. One study showed that 40% of patients abandon prescriptions when they learn the out-of-pocket cost is over $100. That’s why checking the formulary isn’t just about billing-it’s about ethics. You’re not just prescribing a pill. You’re prescribing access.Final Checklist Before You Hit “Send”
Before you finalize any prescription, run through this quick list:- ✅ What’s the patient’s insurance plan name?
- ✅ Is the drug on the formulary?
- ✅ What tier is it? What’s the copay?
- ✅ Does it require PA, ST, or QL?
- ✅ Is there a cheaper, equally effective alternative on Tier 1 or 2?
- ✅ Have you documented your formulary check in the chart?
Do all insurance plans have the same drug list?
No. Each insurer creates its own formulary based on negotiations with drug manufacturers, clinical guidelines, and cost targets. Even two Medicare Part D plans from the same company can have different lists. Always check by the patient’s specific plan.
Can I prescribe a drug not on the formulary?
Yes, but the patient will likely pay full price unless you submit a prior authorization request. Medicare and some commercial plans allow exceptions if you prove medical necessity-like if the patient had an adverse reaction to all formulary alternatives. Medicaid often requires a formal appeal process.
How often are formularies updated?
Medicare Part D plans must notify patients 60 days before any negative change. Most update quarterly-in January, April, July, and October. Commercial insurers may update monthly. Always verify you’re looking at the current version.
What should I do if a patient can’t afford their medication?
First, check if the drug is on a lower tier or if a generic exists. Then, ask if the manufacturer offers a patient assistance program. Many big pharma companies have free or discounted drug programs. Also, contact the insurer’s provider line-they sometimes have emergency overrides for financial hardship.
Are there tools that automate formulary checks?
Yes. EHR systems like Epic and Cerner now include formulary check modules. Starting in 2026, Medicare Part D plans must integrate real-time benefit tools (RTBT) into EHRs, so drug cost and coverage will appear as you type. Until then, use your EHR’s tool if available, or rely on the insurer’s website.

