Many women don’t realize that the first few weeks of pregnancy - when the baby’s heart, brain, spine, and limbs are forming - happen before they even know they’re pregnant. By the time a pregnancy test turns positive, it’s often too late to avoid certain medications that can cause serious birth defects. That’s why creating a medication plan before conception isn’t just smart - it’s essential for a healthy pregnancy.
Why Timing Matters More Than You Think
The most critical window for fetal development is between weeks 3 and 8 after conception. During this time, every organ in the baby’s body is being built. If you’re taking a medication that interferes with this process - even something you’ve used safely for years - it can lead to congenital anomalies like heart defects, cleft palate, or neural tube disorders. Here’s the hard truth: about 45% of pregnancies in the U.S. are unplanned. That means half the time, women are already pregnant before they stop to think about their meds. The solution? Don’t wait. Start reviewing your medications at least 3 to 6 months before you try to conceive. That gives your body time to adjust, your doctor time to switch you to safer options, and your system time to clear out any lingering risks.What Medications Should You Worry About?
Not all drugs are dangerous during pregnancy, but some carry well-documented risks. The biggest red flags include:- Valproic acid (used for seizures and bipolar disorder): Linked to a 10.7% risk of major birth defects, including spina bifida and facial deformities.
- Lithium (for mood disorders): Increases risk of Ebstein’s anomaly, a rare heart defect affecting 1 in 2,000 babies exposed.
- Topiramate (for seizures or migraines): Doubles the risk of oral clefts compared to the general population.
- Methotrexate (for autoimmune diseases like rheumatoid arthritis): Causes miscarriage in up to 18% of cases and severe birth defects.
- Isotretinoin (for severe acne): One of the most dangerous drugs in pregnancy - can cause brain, heart, and ear defects even with short-term use.
- Warfarin (blood thinner): Causes fetal warfarin syndrome with facial and bone abnormalities if taken during the first trimester.
These aren’t hypothetical risks. Data from the Teratology Society and the CDC show exposure to these drugs during early pregnancy can increase the chance of major birth defects by 2 to 10 times.
What’s Safe - and What You Should Start Taking
The good news? Many medications are safe - and some are vital to take before conception.- Folic acid is non-negotiable. For most women, 400-800 mcg daily is enough. But if you have epilepsy, diabetes, obesity, or a family history of neural tube defects, you need 4-5 mg daily. That’s 10 times more than the standard dose - and it cuts the risk of spina bifida by up to 70%.
- Levothyroxine (for hypothyroidism): Your thyroid needs to be perfectly balanced before pregnancy. Aim for a TSH level below 2.5 mIU/L. Once pregnant, you’ll likely need a 30% dose increase. Waiting until you’re pregnant to adjust puts your baby at higher risk for developmental delays and miscarriage.
- Low-molecular-weight heparin (for blood clots): If you’re on warfarin, switch to this before conception. Unlike warfarin, it doesn’t cross the placenta and is safe throughout pregnancy.
- Antiretrovirals (for HIV): If you’re living with HIV, your viral load must be below 50 copies/mL before conception. This reduces the chance of passing HIV to your baby from 25% to less than 1%.
Don’t forget over-the-counter meds and supplements. Some herbal teas, pain relievers like ibuprofen, and even high-dose vitamin A can be risky. Always check with your doctor before continuing anything.

How to Build Your Personal Medication Plan
Creating your plan isn’t just about stopping bad drugs - it’s about building a safer, smarter regimen. Here’s how:- Make a full list of everything you take: prescriptions, OTC meds, vitamins, supplements, and herbal remedies. Include dosages and how often you take them.
- See your doctor at least 6 months before trying to conceive. Bring your list. Ask: “Which of these are safe during pregnancy? Which need to be changed?”
- Get specialist input if you have chronic conditions. A neurologist for seizures, a rheumatologist for lupus or RA, an endocrinologist for thyroid or diabetes - their advice matters.
- Plan for washout periods. Some drugs stay in your system longer than you think. Methotrexate needs 3 months to clear. Isotretinoin requires 1 month of contraception after stopping. Don’t guess - ask for exact timelines.
- Update your contraception. If you’re on seizure meds like carbamazepine, birth control pills may not work. Use a backup method like an IUD or condoms with spermicide.
- Document everything. Use ICD-10 code Z31.69 for your preconception visit - this helps track care and ensures you’re getting the right support.
What If You’re Already Pregnant?
If you’re already pregnant and haven’t reviewed your meds, don’t panic - but act fast. Call your doctor immediately. Many risks are highest in the first 8 weeks, but some medications can still be safely adjusted later. Never stop a drug on your own. Stopping seizure meds or thyroid medication suddenly can be more dangerous than continuing them under supervision.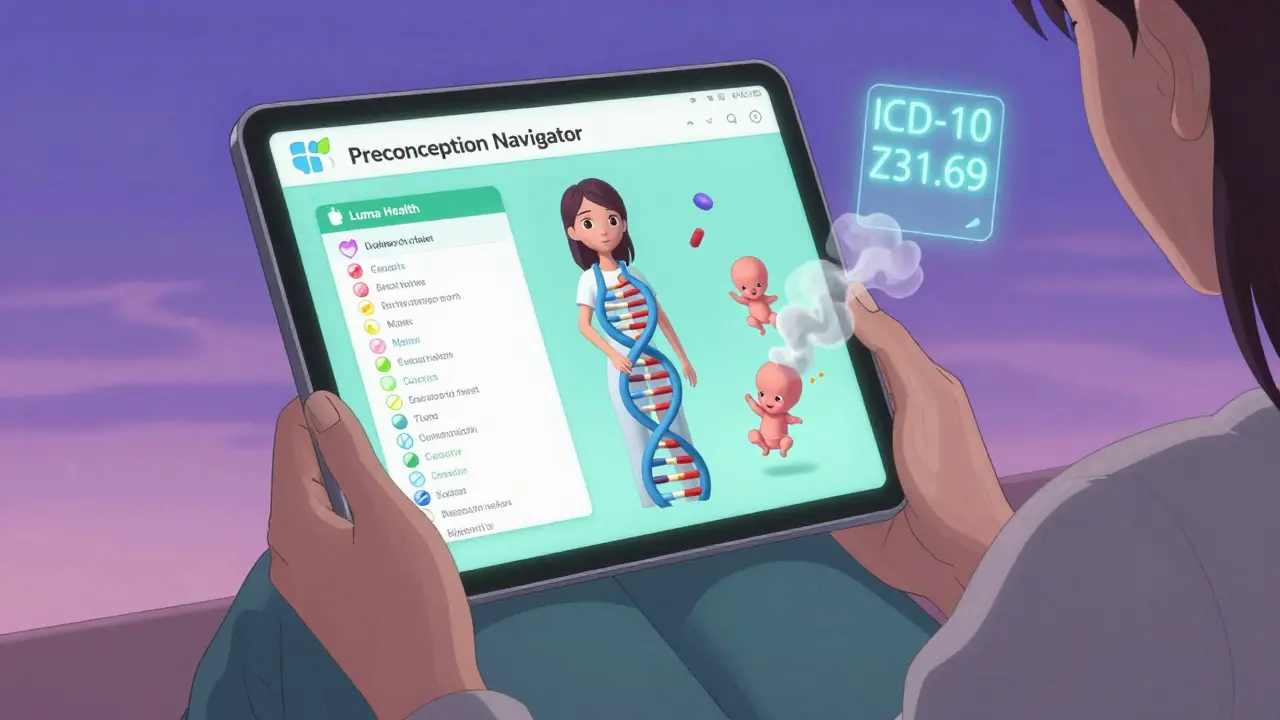
Why Most Women Don’t Get This Care - And How to Change That
Despite all the evidence, only 38% of women with chronic conditions get a preconception medication review. Why? Fragmented healthcare. OB/GYNs often don’t see patients until they’re pregnant. Primary care doctors don’t always ask about pregnancy plans. And many women don’t know they need to bring it up. The solution? Take charge. If you’re thinking about having a baby - even if it’s a year away - schedule a preconception visit. Bring your meds list. Ask the questions. Push for referrals if needed. You’re not being difficult - you’re being responsible.What’s Changing in 2025
New tools are making this easier. In early 2023, the FDA approved the first digital tool - Luma Health’s Preconception Navigator - that uses AI to scan your meds against a database of over 1,200 teratogens. It flags risks and suggests alternatives in seconds. More clinics are starting to use it. Also, guidelines now include women with higher BMI. If your BMI is 30 or above, you should stop weight-loss drugs like liraglutide at least 2 months before trying to conceive - there’s not enough safety data yet. And research is moving toward personalized risk scores. The NIH’s PharmaTox study is testing whether combining your genetics, metabolism, and medication history can predict exactly how a drug will affect your future baby. That’s the future - and it’s coming fast.Bottom Line: Do This Now
If you’re planning a pregnancy, your medication plan isn’t optional. It’s the first step to giving your baby the best possible start.- Start 6 months before trying.
- Review every pill, patch, and supplement.
- Switch risky drugs now - don’t wait.
- Take high-dose folic acid.
- Get specialist input if you have a chronic condition.
Every day you wait increases the chance your baby will be exposed to something harmful during the most vulnerable time. You can’t control everything - but you can control your meds. Do it before you conceive.
Do I need to stop all my medications before getting pregnant?
No - not all medications need to be stopped. Many are safe to continue during pregnancy, like levothyroxine, certain antidepressants, and insulin. The goal isn’t to stop everything - it’s to replace the risky ones with safer alternatives. Always work with your doctor to make changes gradually and safely.
How long before conception should I start planning?
At least 3 to 6 months. Some drugs, like methotrexate or isotretinoin, take months to fully leave your system. Starting early gives you time to adjust your treatment, monitor your health, and ensure you’re in the best possible condition before conception.
Is folic acid really that important?
Yes - extremely. Folic acid reduces the risk of neural tube defects like spina bifida by up to 70%. The standard dose (400-800 mcg) works for most women, but if you have epilepsy, diabetes, or a previous affected pregnancy, you need 4-5 mg daily. Don’t rely on prenatal vitamins alone - check the label to make sure you’re getting enough.
Can I take herbal supplements while planning pregnancy?
Many herbal supplements haven’t been tested for safety in pregnancy. Some, like black cohosh or dong quai, can stimulate the uterus or interfere with hormones. Others, like high-dose vitamin A, are directly toxic to the developing fetus. Always tell your doctor what herbs or supplements you’re taking - don’t assume they’re safe just because they’re natural.
What if my doctor doesn’t mention preconception planning?
Take the lead. Doctors are busy, and many don’t routinely bring up preconception care unless you’re actively trying. Don’t wait for them to ask. Say: “I’m thinking about getting pregnant in the next year - can we review my medications?” Bring a list. Ask specific questions. Your health - and your future baby’s - depends on it.
Are there any new medications approved for use before pregnancy?
The FDA’s 2023 Pregnancy and Lactation Labeling Rule requires newer drugs to include clearer safety data, but most existing medications still use outdated risk categories. The real breakthrough is in digital tools like Luma Health’s Preconception Navigator, which helps doctors quickly identify safe alternatives. Newer antiseizure drugs like lamotrigine and levetiracetam are now preferred over valproic acid because they’re much safer in early pregnancy.

