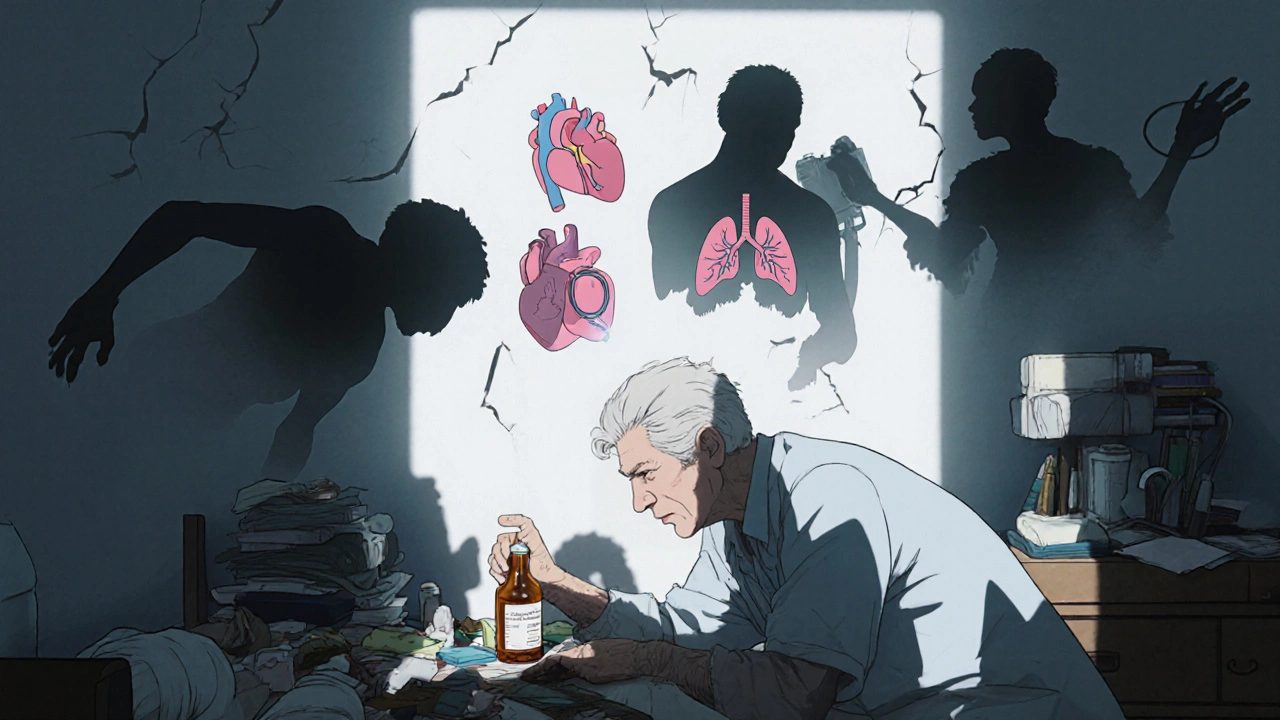
A cough in an older adult isn’t just a nuisance-it can be a warning sign. While a dry cough might pass in a few days for a child, in someone over 65, it can signal something serious: pneumonia, heart failure, or even a reaction to common blood pressure meds. The body’s defenses weaken with age. Swallowing becomes slower. Lungs lose elasticity. Cough reflexes dull. That’s why a cough that seems mild to you could be a red flag for your parent or grandparent.
Know when a cough needs urgent care
Not every cough needs a doctor. But some do-right away. If an elderly person has a cough with any of these, call a doctor or go to urgent care:
- High fever (over 38.5°C) that won’t break
- Coughing up blood or thick, dark mucus
- Shortness of breath even when sitting still
- Chest pain that feels like pressure or tightness
- Confusion, dizziness, or sudden weakness
- Cough lasting more than three weeks without improvement
These aren’t just "old age" symptoms. They’re signs the body is struggling. A 2023 study in the Journal of the American Geriatrics Society found that over 40% of seniors hospitalized for pneumonia had been dismissed earlier with a simple "it’s just a cold" diagnosis. Don’t wait. If in doubt, get it checked.
Why common cough medicines can be dangerous
Many older adults reach for over-the-counter cough syrups or pills because they’re easy to get. But many contain ingredients that are risky for seniors.
Dextromethorphan, found in brands like Robitussin DM, can cause dizziness, confusion, or even hallucinations in older people. Pseudoephedrine, used in decongestants, raises blood pressure and can trigger heart rhythm problems. Antihistamines like diphenhydramine (Benadryl) are linked to increased risk of falls and memory issues.
The American College of Chest Physicians advises against using these in people over 65 unless closely monitored by a doctor. Many pharmacies now flag these drugs for seniors automatically-but not all do. Always ask: "Is this safe for someone my age?"
Safe, effective home remedies
When the cough isn’t dangerous, focus on comfort and support-not suppression. Here’s what actually works:
- Hydration - Water, broth, herbal tea. Thick mucus is harder to clear. Keeping fluids up thins it out. Aim for 6-8 glasses a day unless restricted by heart or kidney issues.
- Honey - One teaspoon before bed helps reduce nighttime coughing. A 2020 Cochrane review found honey was as effective as dextromethorphan for kids and safer for seniors. Don’t give honey to anyone with diabetes without checking with their doctor first.
- Humidifiers - Dry air irritates airways. A cool-mist humidifier in the bedroom at night adds moisture. Clean it daily to prevent mold. If you don’t have one, run a hot shower and sit in the steamy bathroom for 10 minutes.
- Elevate the head - Use an extra pillow or wedge under the mattress. Lying flat lets mucus pool in the throat, triggering coughing. Raising the head even 6 inches helps.
- Warm saltwater gargle - For a scratchy throat, mix half a teaspoon of salt in warm water. Gargle for 30 seconds, spit. Do this twice a day.
These aren’t magic cures. But they reduce irritation, help the body clear mucus naturally, and avoid dangerous side effects.
Watch for silent coughs and hidden causes
Some coughs in older adults don’t sound loud. They’re dry, tickly, or just a throat-clearing habit. These are often missed.
One common culprit: ACE inhibitors. These are blood pressure pills like lisinopril or enalapril. Up to 20% of people taking them develop a persistent dry cough. It’s not an allergy-it’s a side effect. The cough doesn’t respond to cough medicine. It only stops when the drug is switched to a different class, like an ARB (e.g., losartan). If an elderly person started a new blood pressure med and then got a cough, this is likely the cause.
Another hidden cause: GERD (gastroesophageal reflux). Stomach acid creeping up the throat irritates it, especially at night. People might not feel heartburn-they just cough. Try avoiding large meals after 6 p.m., don’t lie down for 3 hours after eating, and elevate the head of the bed. If it persists, ask a doctor about a trial of acid-reducing meds.
And don’t forget lung conditions. COPD, asthma, and even early-stage lung cancer can start with a cough. If it’s been there for months, even if it’s "just a little," get a chest X-ray or spirometry test.
When to use prescribed treatments
Some coughs need medical help-not just home care.
If the cough comes with wheezing or tightness, it might be asthma or COPD flare-up. Inhaled bronchodilators like albuterol can help. If mucus is thick and green or yellow, it could be a bacterial infection. Antibiotics might be needed-but only if confirmed by a doctor. Don’t self-prescribe.
For chronic coughs with no clear cause, doctors may prescribe low-dose inhaled corticosteroids or gabapentin. These aren’t first-line, but they’ve helped many seniors with nerve-related coughs. Always start low and go slow.
Remember: antibiotics don’t work on viruses. Most coughs are viral. Overusing antibiotics leads to resistance and side effects like diarrhea or yeast infections-both dangerous for older adults.

Prevention is part of management
Stopping a cough before it starts is better than treating it.
- Vaccines - Get the yearly flu shot and the pneumococcal vaccine (PCV20 or PPSV23). These are recommended for everyone over 65. They don’t prevent all coughs, but they cut hospitalizations by up to 60%.
- Handwashing - Germs spread fast. Use soap and water for 20 seconds. Alcohol gel works too.
- Avoid smoke - Even secondhand smoke irritates aging lungs. No smoking indoors. Keep away from crowded places during cold and flu season.
- Stay active - Walking daily, even 15 minutes, helps keep lungs clear. Inactivity leads to mucus buildup.
One simple trick: drink warm fluids after meals. It helps clear mucus from the throat and reduces post-meal coughing. Many seniors notice a big difference just by doing this.
What to do if the cough won’t go away
If the cough lasts longer than four weeks, it’s time for a full review. Ask the doctor for:
- A chest X-ray
- Pulmonary function test (spirometry)
- Review of all medications
- Referral to a pulmonologist or ENT if needed
Don’t accept "it’s just old age" as an answer. Persistent cough is not normal. It’s a signal. And seniors deserve to have their signals heard.
Is honey safe for elderly people with diabetes?
Honey raises blood sugar, so people with diabetes should use it cautiously. A teaspoon occasionally may be fine, but it’s not risk-free. Always check with a doctor or dietitian first. There are safer alternatives like sugar-free cough drops or warm herbal teas with lemon.
Can a cough be caused by heart problems?
Yes. Heart failure can cause fluid to back up into the lungs, leading to a persistent cough, especially when lying down. This cough is often dry or produces white, frothy mucus. If an elderly person coughs more at night or when resting, and also has swollen ankles or shortness of breath, heart failure should be ruled out.
Should I give my elderly parent cough syrup from my medicine cabinet?
No. Many adult cough syrups contain ingredients that are unsafe for seniors, like pseudoephedrine or diphenhydramine. Even if it worked for you, it could cause confusion, falls, or high blood pressure in an older person. Always check with a pharmacist or doctor before giving any OTC medicine to someone over 65.
How long is too long for a cough in an elderly person?
A cough lasting more than three weeks should be evaluated. If it’s been four weeks or longer, even if it’s mild, it’s not normal. Chronic cough in seniors often signals an underlying condition like GERD, medication side effects, or lung disease. Don’t wait-it’s worth a doctor’s visit.
Do humidifiers help with coughs in older adults?
Yes, especially in dry climates or during winter. Dry air makes the throat and airways irritated, worsening coughs. A cool-mist humidifier adds moisture and can reduce coughing at night. But it must be cleaned daily to prevent mold, which can trigger breathing problems. Avoid warm-mist humidifiers-they’re a breeding ground for bacteria.
Final thoughts: Listen to the body
A cough in an elderly person isn’t something to ignore. It’s the body’s way of saying something’s off. Sometimes it’s harmless. Sometimes it’s serious. The key is knowing the difference-and acting early.
Keep track: when did it start? What makes it better or worse? Is there mucus? Any other symptoms? Write it down. Bring it to the doctor. Don’t assume it’s just aging. Seniors deserve better than that.
Simple steps-hydration, honey, humidifiers, avoiding risky meds-can make a real difference. But when in doubt, get it checked. One visit could prevent a hospital stay. And that’s worth the effort.

