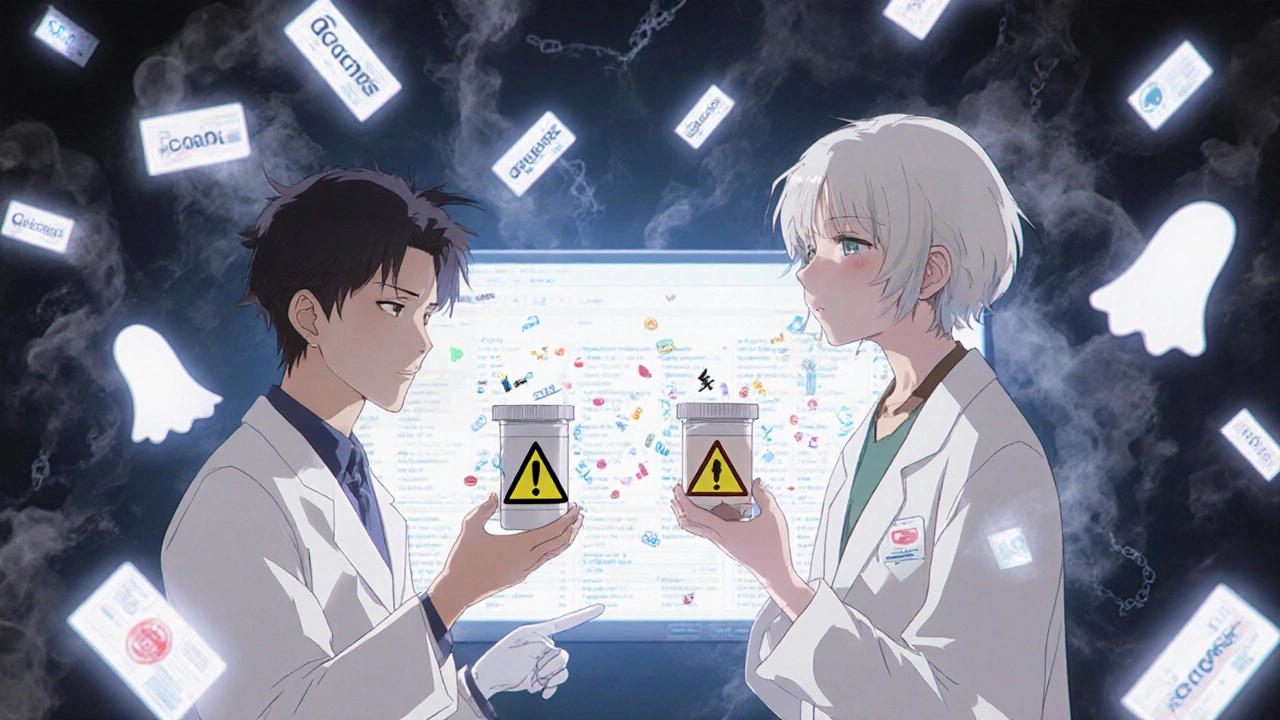
Switching from a brand-name drug to a generic version can save you hundreds of dollars a month. But sometimes, people swear the generic doesn’t work the same. They feel more tired, get stomach upset, or notice their anxiety flaring up. It’s not all in their head. The issue isn’t the active ingredient-it’s what’s hiding in the pill: the inactive ingredients.
What Are Inactive Ingredients, Really?
Inactive ingredients, also called excipients, are the non-medicine parts of your pill. They don’t treat your condition. But they do a lot of heavy lifting behind the scenes. They hold the tablet together. They help it dissolve in your stomach. They make it easier to swallow. They keep it from going bad on the shelf.
Common ones include lactose (a milk sugar), microcrystalline cellulose (ground wood pulp), starch, dyes, preservatives like sodium benzoate, and coatings made from things like hydroxypropyl methylcellulose. You won’t find these on the box label as ‘active.’ But they’re there-sometimes in dozens of different forms across different brands.
Think of it like baking cookies. Two recipes can both have chocolate chips as the main ingredient, but one uses butter, another uses margarine. One has sea salt, another has table salt. The taste changes. The texture changes. The cookies aren’t the same, even if the chocolate is identical.
Why the FDA Allows Differences
The U.S. Food and Drug Administration (FDA) requires generics to have the same active ingredient, strength, dosage form, and route of administration as the brand-name drug. They must also prove they’re bioequivalent-meaning your body absorbs the medicine at nearly the same rate and amount.
That bioequivalence standard? The 90% confidence interval for absorption must fall between 80% and 125% of the brand-name version. That sounds loose, but in practice, most generics are within 3-4% of the original. So why do people still feel different?
Because bioequivalence doesn’t care about fillers. It doesn’t test how you feel after swallowing the pill. It doesn’t check if you get a headache from a dye or bloating from lactose. The FDA only cares that the medicine works. And for most people, it does.
Who’s Most Likely to Notice a Difference?
Studies show that about 95% of people notice zero difference when switching to a generic. But 1-2% do. And for those people, the problem is almost always the inactive ingredients.
People with:
- Lactose intolerance (about 36% of Americans) might get bloating or diarrhea from generics using lactose as a filler. Around 40% of oral meds contain it.
- Gluten sensitivity might react to starches derived from wheat-even if the label says ‘gluten-free,’ the source isn’t always disclosed.
- Sulfite allergies (3-10% of asthmatics) could have breathing issues from preservatives in liquid or injectable generics.
- Dye sensitivities might get rashes or headaches from red #40, yellow #5, or other colorants used to make pills look different from the brand.
- Narrow therapeutic index conditions like thyroid disease (levothyroxine), epilepsy (phenytoin), or heart failure (digoxin) can be more sensitive to even tiny changes in how the drug is released. A 5% shift in absorption can push levels out of the safe range.
One patient on PatientsLikeMe reported her TSH levels jumped after switching to a generic levothyroxine. Her doctor had to switch her back. Another Reddit user said their sertraline generic caused constant nausea-something the brand never did. Both cases point to excipients, not the drug itself.

Cost vs. Comfort: The Real Trade-Off
Brand-name Lipitor costs around $370 a month. The generic? About $4. That’s not a typo. That’s the power of generics.
Across the U.S., generics make up 90% of prescriptions but only 23% of drug spending. Over the last decade, they’ve saved the system over $2 trillion.
But money isn’t everything. For someone with chronic pain, anxiety, or a thyroid disorder, feeling stable matters more than saving $300. If a generic makes you feel worse, the cost savings don’t matter.
That’s why some manufacturers now offer ‘authorized generics’-made by the original brand company, but sold under a generic label. They’re identical in active and inactive ingredients. They cost less, but not as much as standard generics. They’re growing fast, making up about 15% of the generic market now.
What You Can Do If You Suspect a Problem
If you switch to a generic and feel off, don’t assume it’s ‘all in your head.’ Track it.
- Keep a journal for 2-4 weeks. Note when you take the pill, what you ate, your mood, energy, sleep, and any side effects.
- Check the label. Look up the inactive ingredients. You can find them on the pharmacy’s website or ask for the full list.
- Compare to your old pill. Did the new one have a different color? Shape? Marking? That’s a clue it’s a different formulation.
- Ask your pharmacist. They can tell you which manufacturer made your generic-and whether it’s the same one you were on before.
- Ask your doctor about switching to an authorized generic or a different generic brand. Not all generics are made the same.
Pharmacists spend 5-10 minutes reviewing inactive ingredients when patients report issues. They’ve seen this before. They can help.
The Future: Better Labels, Fewer Surprises
The FDA is starting to pay more attention. In 2023, they issued new draft guidance for generics of high-risk drugs like levothyroxine and warfarin. They’re also planning to expand their Inactive Ingredient Database in early 2024. That means you’ll soon be able to look up any drug and see every single excipient it contains-down to the exact amount.
More manufacturers are responding too. ‘Clean label’ generics are popping up-no artificial dyes, no lactose, no preservatives. These are still rare, but they’re growing. By 2025, an estimated 70% of generic makers plan to offer allergen-free versions of common medications.
It’s not about rejecting generics. It’s about making them safer for everyone.
Bottom Line: Generics Work-But Not Always the Same Way
For 95 out of 100 people, switching to a generic is a no-brainer. You save money. You get the same medicine. No downside.
But for the other 5? The difference isn’t in the active ingredient. It’s in the fillers, the dyes, the coatings. And those matter.
If you’ve noticed a change after switching, you’re not imagining it. Talk to your pharmacist. Check the ingredients. Don’t settle for feeling worse just because it’s cheaper. Your health isn’t a cost-cutting exercise. It’s personal. And you deserve a medication that works-not just in theory, but in your body, too.