Hepatitis C Treatment Regimen Comparison Tool
Compare Treatment Options
Select filters above to see how different treatment options compare. You can filter by genotype coverage, cure rates, or cost to find the best option for your setting.
Treatment Regimen Comparison
| Regimen | Genotype Coverage | SVR-12 Rate | Typical Cost (USD) | Monitoring Needs |
|---|---|---|---|---|
| Ledipasvir + Sofosbuvir (Generic) | 1-4 (pangenotypic) | 95-98% | $300-450 | Baseline labs, end-of-treatment tests |
| Sofosbuvir + Ribavirin | 1,2,3 (limited for genotype 3) | 80-90% | $350-500 | Frequent hemoglobin monitoring |
| Pegylated Interferon + Ribavirin | All (low efficacy for genotype 1) | 40-60% | $150-250 | Monthly injections, extensive labs |
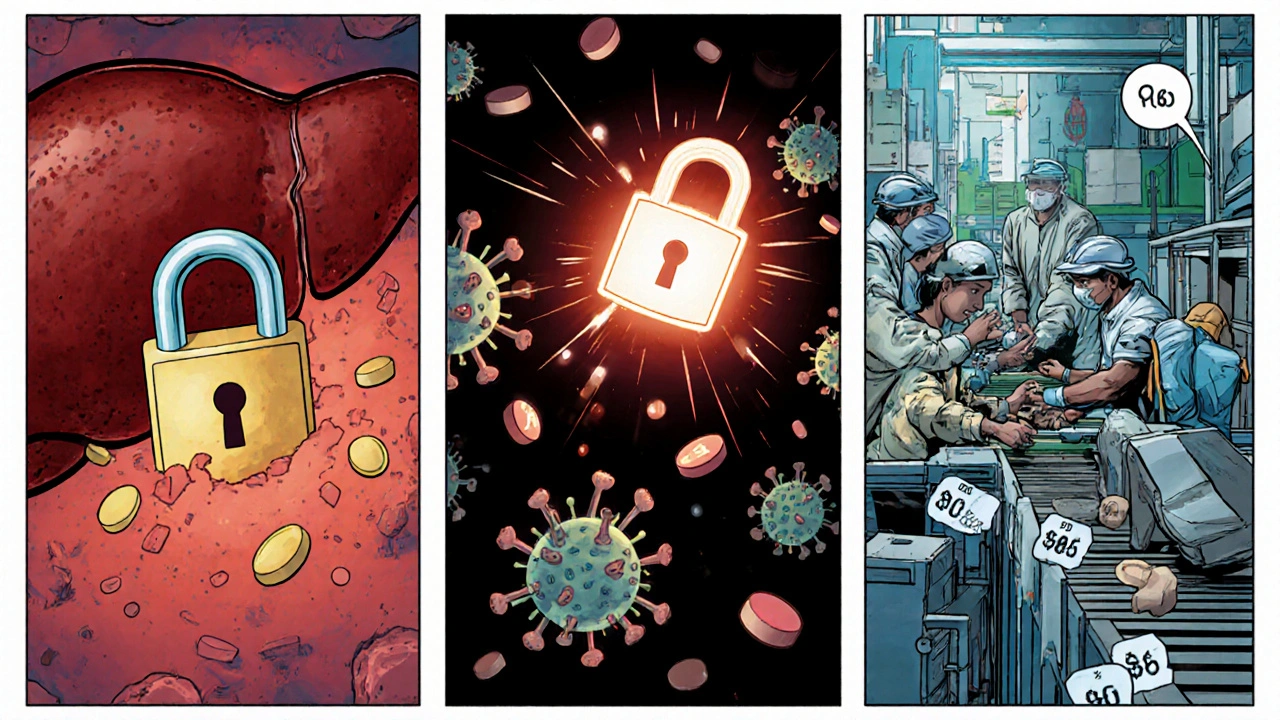
When hepatitis C hits a community with scarce medical supplies, the outcome often looks bleak. Ledipasvir is a direct‑acting antiviral (DAA) that has reshaped that picture for many low‑income regions.
What is Ledipasvir?
Ledipasvir is a nucleotide‑binding inhibitor that targets the NS5A protein of hepatitis C virus (HCV). It was first approved in the United States in 2014 as part of the combination product Harvoni. The drug’s small‑molecule design lets it halt viral replication inside liver cells, delivering cure rates above 95% in clinical trials.
Understanding HepatitisC
Hepatitis C is a blood‑borne infection that can lead to chronic liver disease, cirrhosis, and liver cancer if untreated. The World Health Organization estimates that over 58million people live with chronic HCV worldwide, and a large share resides in low‑ and middle‑income countries where access to modern therapy is limited.
How Ledipasvir Works Against the Virus
The NS5A protein is essential for assembling new viral particles. By binding to this protein, Ledipasvir blocks the formation of the viral replication complex, dramatically reducing viral load within weeks. When paired with Sofosbuvir - a polymerase inhibitor - the duo attacks two critical steps in the HCV life cycle, creating a potent, pangenotypic regimen.
Clinical Evidence in Resource‑Limited Environments
Several open‑label studies have focused on sub‑Saharan Africa, South‑East Asia, and Eastern Europe, where generic versions of the Ledipasvir/Sofosbuvir combo are produced under voluntary licences. In the “GENERIC‑C” trial (2023), 1,025 patients received 12‑week therapy with cure rates (sustained virologic response, SVR‑12) of 96% across genotypes 1‑4. Importantly, adverse‑event rates were under 5%, and treatment discontinuation was rare.
Cost and Access Challenges
The original brand price exceeded US$94,000 for a 12‑week course, a figure impossible for most national health budgets. However, after the 2017 voluntary licence agreements, generic manufacturers in India and Egypt began offering the combo at US$300-$450 per course. The World Health Organization (WHO) incorporated this price point into its 2024 Model List of Essential Medicines, urging governments to negotiate bulk purchases.
Key cost‑driving factors include:
- Manufacturing scale - high‑volume production reduces per‑tablet cost.
- Patent pool participation - allows multiple firms to compete.
- Supply‑chain logistics - efficient distribution lowers wastage.
Comparing Treatment Options for Low‑Resource Settings
| Regimen | Genotype Coverage | SVR‑12 Rate | Typical Cost (USD) | Monitoring Needs |
|---|---|---|---|---|
| Ledipasvir+Sofosbuvir (Harvoni) | 1‑4 (pangenotypic with dose adjustment) | 95‑98% | 300‑450 (generic) | Baseline labs, end‑of‑treatment tests |
| Sofosbuvir+Ribavirin | 1,2,3 (limited for genotype3) | 80‑90% | 350‑500 | Frequent hemoglobin monitoring |
| Pegylated Interferon+Ribavirin | All (low efficacy for genotype1) | 40‑60% | 150‑250 | Monthly injections, extensive labs |
The Ledipasvir/Sofosbuvir combo stands out for its high cure rate, short treatment duration, and minimal side‑effects, making it ideal for clinics with limited staffing and lab capacity.

Implementation Strategies for Low‑Income Health Systems
Success hinges on three practical pillars:
- Negotiated Procurement - Governments should pool demand regionally, leveraging WHO’s generic licence to secure bulk discounts.
- Task‑Shifting to Community Health Workers - With a once‑daily oral regimen, non‑physician staff can supervise adherence, conduct brief symptom checks, and flag any adverse events.
- Point‑of‑Care Viral Load Testing - Portable PCR platforms (e.g., GeneXpert) reduce the need for centralized labs, allowing on‑site confirmation of SVR‑12.
Case studies from Rwanda and Myanmar show that integrating these steps can cut treatment initiation time from months to weeks.
Key Takeaways Checklist
- Ledipasvir targets the NS5A protein, delivering >95% cure rates.
- Generic pricing (US$300‑450) meets WHO’s essential‑medicine criteria.
- Compared to older interferon‑based regimens, it eliminates injections and severe side‑effects.
- Bulk procurement and task‑shifting are proven cost‑saving tactics.
- Portable viral‑load testing accelerates treatment monitoring in remote clinics.
Frequently Asked Questions
Can Ledipasvir be used for all HCV genotypes?
The standard Ledipasvir/Sofosbuvir regimen covers genotypes1‑4 effectively. For genotype3, a higher dose or addition of ribavirin is sometimes recommended.
Is the drug safe for pregnant women?
Current data are limited; the WHO advises postponing DAA therapy until after delivery unless the maternal health risk outweighs potential fetal exposure.
How do I ensure adherence in a remote village?
Use simple pill‑boxes, schedule weekly check‑ins with community health volunteers, and provide visual reminders (e.g., stickers) on medication bottles.
What are the main barriers to scaling up treatment?
High upfront drug costs, limited laboratory capacity for baseline screening, and regulatory bottlenecks for generic imports are the top hurdles.
Where can I find up‑to‑date pricing information?
The WHO Medicines Price Information (MPHI) portal publishes quarterly updates on generic DAA prices worldwide.

