Migraine with Aura Birth Control Risk Calculator
This tool helps you assess your stroke risk if you have migraine with aura and are considering estrogen-based birth control. Based on your inputs, it will provide a risk score and recommendations.
Important: This tool is for informational purposes only and should not replace professional medical advice. Always consult with your healthcare provider before making birth control decisions.
If you get migraines with aura-flashing lights, blind spots, tingling in your hands, or speech trouble before your headache starts-your birth control choices matter more than you might think. For years, doctors have told women with this type of migraine to avoid any birth control with estrogen. But today, with newer, lower-dose pills on the market, that advice is being questioned. So what’s the real risk? And what should you do if you need reliable birth control but also suffer from migraines with aura?
What Exactly Is Migraine with Aura?
Migraine with aura isn’t just a bad headache. It’s a neurological event. Before the pain hits, you might see zigzag lines, stars, or blind spots in your vision. Some people feel numbness on one side of their face or hand. Others struggle to speak clearly. These symptoms usually last 5 to 60 minutes and then fade, followed by the headache. Not all migraine symptoms count as aura. Nausea, sensitivity to light, or feeling tired beforehand? Those are warning signs, not aura. Only focal neurological symptoms-things that affect specific parts of your brain-qualify.
That distinction is critical. Women with migraine without aura can often use estrogen-based birth control safely. But with aura? The risk profile changes. And that’s where the controversy begins.
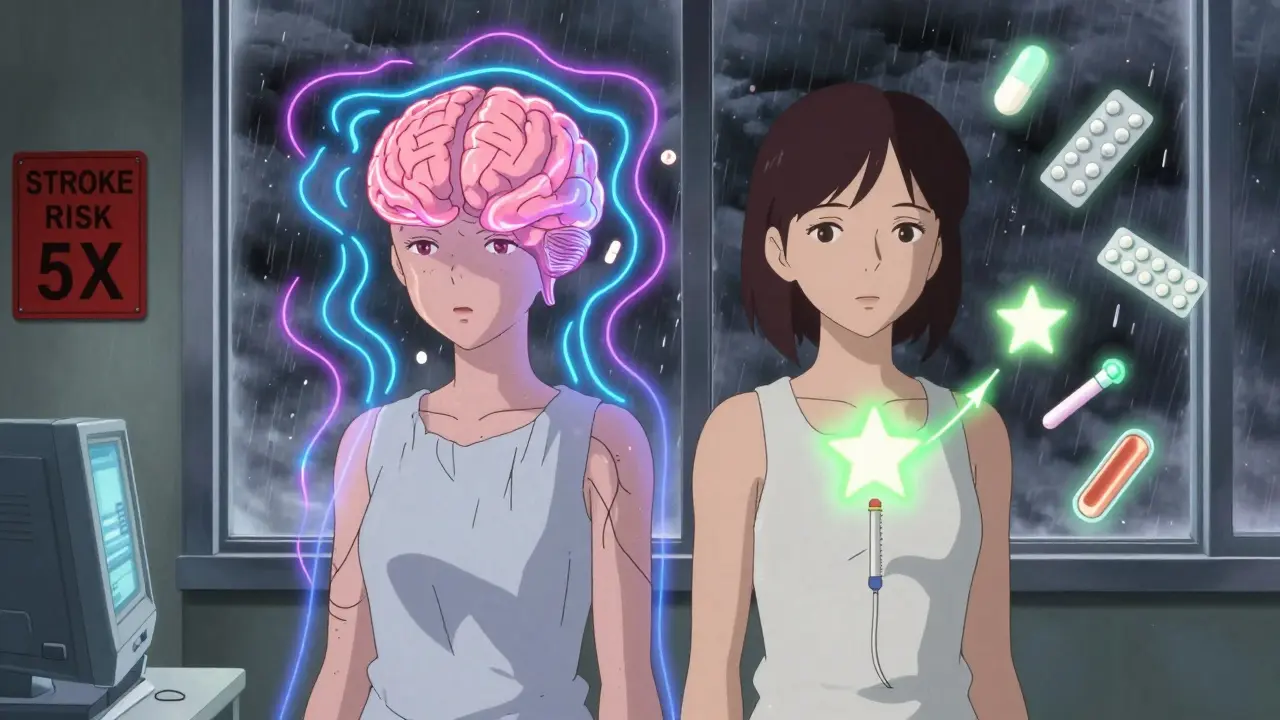
Why Estrogen Raises Stroke Risk
Estrogen in birth control pills thickens the blood slightly and can make clots more likely. For most young, healthy women, that’s not a big deal. But add migraine with aura into the mix, and your stroke risk jumps. According to the Reproductive Access Organization (2023), healthy women under 35 have about a 6 in 100,000 chance of having an ischemic stroke each year. For women with migraine with aura who take estrogen-containing pills, that number rises to about 30 in 100,000-five times higher.
The World Health Organization (WHO) says this risk is too high. Their guidelines, updated in 2019, list estrogen-containing birth control as absolutely contraindicated for women with migraine with aura. The CDC backs this up, saying the combination of estrogen and aura increases stroke risk sixfold compared to having neither factor.
But here’s the twist: most of this data comes from older, high-dose pills-think 50 micrograms of ethinyl estradiol or more. Today’s pills are different. Many contain only 20 to 35 micrograms. Some ultra-low-dose options have as little as 10 to 15 micrograms. And new research suggests those lower doses might not carry the same danger.
The New Evidence: Are Low-Dose Pills Safer?
Dr. Pinar Batur’s 2022 study, published by the American Migraine Foundation, looked at 127 women with migraine with aura who had strokes. She found that stroke risk didn’t spike as much as expected in women using low-dose estrogen pills. Her takeaway? The old warnings might be based on outdated data.
Dr. Anne Calhoun at Stanford Medicine agrees. In her 2017 review, she pointed out that modern ultra-low-dose pills may not raise stroke risk at all-and might even reduce aura frequency. If your migraines happen less often, your stroke risk goes down. That’s a powerful idea: birth control could help manage your migraines, not just prevent pregnancy.
But here’s the catch. Batur’s study only included 127 stroke cases. That’s not enough to draw firm conclusions. And the WHO, CDC, and American College of Obstetricians and Gynecologists (ACOG) still stand by their strict warnings. Why? Because stroke is rare but devastating. One mistake can change your life.
Frequency Matters: How Often Do You Get Migraines?
Not all migraine with aura is the same. If you have a few attacks a year, your risk is lower than if you have them weekly. Research from the NIH shows a J-shaped curve: risk goes up if you have migraines less than once a month, and again if you have them once a week or more. Monthly attacks? No significant increase in stroke risk.
And if you have more than 12 migraines a year with aura? Your stroke risk jumps even higher. One study found an odds ratio of 10.4-meaning you’re over ten times more likely to have a stroke than someone without frequent aura.
That’s why doctors don’t just look at whether you have aura-they look at how often it happens. And they check for other risk factors: Do you smoke? Are you over 35? Do you have high blood pressure or diabetes? Family history of stroke? Each of these adds up.
What Are Your Alternatives?
If estrogen is off the table, you still have plenty of safe, effective options.
- Progestin-only pills (the “mini-pill”)-no estrogen, no added stroke risk.
- Levonorgestrel IUD-lasts 3 to 8 years, releases tiny amounts of hormone locally. No systemic estrogen.
- Etonogestrel implant-a small rod under your skin, effective for 3 years.
- Depo-Provera shot-every 3 months, no estrogen.
- Copper IUD-completely hormone-free, works for up to 12 years.
- Barrier methods-condoms, diaphragms-less effective but zero hormonal risk.
The American College of Obstetricians and Gynecologists (ACOG) specifically recommends these for women with migraine with aura, especially if they’re over 35 or smoke. These methods don’t increase stroke risk. Period.
When Might Estrogen Still Be an Option?
Some doctors are starting to consider low-dose estrogen pills for select patients-only if:
- You’re under 35
- You don’t smoke
- Your blood pressure is normal
- You have fewer than 12 migraines a year
- You’re using a pill with 20-25 micrograms of estrogen or less
- You’ve had no aura symptoms in the past year
Even then, it’s not a blanket approval. It’s a careful, individualized decision. You need to know the signs of stroke: sudden numbness, confusion, trouble speaking, vision loss, dizziness, or a severe headache with no known cause. If any of those happen, stop the pill and get help immediately.

What About Menstrual Migraines?
Many women with migraine with aura get them right before or during their period. That’s called menstrual migraine. For some, estrogen drops trigger the attack. Continuous birth control-skipping the placebo week-can prevent that drop and reduce migraine frequency. That’s why some women with aura want estrogen pills: they’re not just avoiding pregnancy-they’re avoiding pain.
But here’s the trade-off. If you’re willing to try continuous low-dose estrogen to reduce aura, you’re also accepting a small, uncertain stroke risk. For many, the benefit of fewer migraines outweighs the risk. For others, it doesn’t. That’s why shared decision-making matters. Your doctor shouldn’t just tell you “no.” They should help you weigh the pros and cons based on your life, your goals, and your numbers.
What Should You Do Next?
Don’t stop your birth control cold. Don’t switch to something new without talking to your doctor. Here’s what to do:
- Track your migraines for at least 3 months. Note frequency, aura symptoms, duration, and triggers.
- Get your blood pressure checked. If it’s above 140/90, estrogen is not safe.
- Quit smoking if you smoke. Smoking with aura and estrogen is a dangerous combo.
- Ask your doctor: “Do I have migraine with aura, or just a bad headache?” Get it confirmed.
- Discuss progestin-only options first. They’re safer and just as effective.
- If you still want estrogen, ask about low-dose pills (20-25 mcg ethinyl estradiol) and whether you qualify based on your risk profile.
The bottom line? Migraine with aura and estrogen birth control don’t mix for most women. But medicine isn’t black and white. With better data, smarter pills, and more personalized care, some women might find a safe middle ground. But it takes honesty, tracking, and a doctor who listens.
When to Seek Immediate Help
If you’re on any hormonal birth control and suddenly experience:
- Weakness or numbness on one side of your body
- Slurred speech or trouble understanding others
- Sudden vision loss in one or both eyes
- A headache unlike any you’ve had before-especially if it’s the worst of your life
- Severe dizziness or loss of balance
Call emergency services immediately. These could be signs of a stroke. Don’t wait. Don’t assume it’s just a migraine. Time is brain.