For decades, doctors told patients to take statins at night. The logic was simple: your body makes the most cholesterol while you sleep. So, if you take a statin before bed, it hits hardest when it matters most. But today, that advice doesn’t hold for most people. The real question isn’t whether to take your statin at night or in the morning-it’s whether you’ll actually remember to take it at all.
Why Night Was the Old Standard
Back in the 1980s, when statins like simvastatin and lovastatin first hit the market, scientists noticed something important. Cholesterol production in the liver peaks between midnight and 4 a.m. That’s when your body’s natural machinery, called HMG-CoA reductase, goes into overdrive. The early statins had short half-lives-meaning they cleared out of your system quickly. Simvastatin lasts just 1.9 to 3 hours. Lovastatin? Even less. So if you took them in the morning, by the time your liver ramped up cholesterol production at night, the drug was already gone. That’s why doctors said: take it at bedtime. It made sense. Studies backed this up. One 1995 trial showed that taking simvastatin at night lowered LDL (bad cholesterol) by 13.4% more than taking it in the morning. Another study found that a 5mg dose of simvastatin taken at night cut cholesterol by 21%, while the same dose taken in the morning only cut it by 14%. That’s a 50% relative improvement. For patients on these older statins, timing wasn’t just helpful-it was critical.But Most Statins Today Are Different
Here’s the twist: the statins you’re likely taking now aren’t the same ones from 20 years ago. Today, about 82% of new statin prescriptions are for long-acting versions like atorvastatin (Lipitor), rosuvastatin (Crestor), and pitavastatin (Livalo). These drugs stick around in your bloodstream for 12 to 20 hours. That means whether you take them at 7 a.m. or 11 p.m., your liver still gets a steady dose of the drug all night long. A 2017 analysis of 17 studies involving over 3,300 people found that for long-acting statins, the difference in LDL reduction between morning and evening dosing was tiny-just 0.4% to 2.3%. That’s less than the natural daily variation in cholesterol levels. In practical terms? It’s not meaningful. If your LDL drops from 160 to 120, and then drops to 118 instead of 119 because you took it at night, you’re not getting better protection. You’re just getting a fraction of a point.Side Effects Don’t Care About Timing
A lot of people worry that taking statins at night might cause more side effects-muscle pain, liver issues, or even a higher risk of diabetes. But data says otherwise. The FDA’s own adverse event database, covering over 4.2 million statin prescriptions, found no difference in side effect rates between morning and evening dosing. Muscle pain? Same rate. Liver enzyme spikes? No difference. New-onset diabetes? No link to timing. Even the most common complaint-myalgia, or muscle aches-shows no pattern based on when you take the pill. One 2021 study of 12,000 patients found that those taking statins at night had slightly more reports of muscle discomfort, but the difference vanished when researchers adjusted for age, activity level, and other factors. In short: if you feel sore, it’s not because of the clock. It’s probably your body’s reaction to the drug itself.
What Actually Makes a Difference: Adherence
This is where the real story lies. A 2019 study from the Mayo Clinic tracked 12,498 statin users. Those told to take their meds at night had a medication possession ratio (MPR) of 0.87. Those taking them in the morning? 0.98. That means night-takers missed about 2.1 more doses per month. Why? Life happens. People work late. Travel. Forget. Sleep in. Or, like one Reddit user put it: “I kept forgetting my simvastatin at night. My doctor switched me to morning rosuvastatin. My LDL actually improved because I never miss a dose now.” Another study found that patients given a simple smartphone reminder to take their statin at 8 a.m. had a 92% adherence rate. Those told to take it at night without reminders? Only 76%. The morning group ended up with nearly the same LDL reduction as the night group-even though the night group was supposed to be more effective. The only real difference? Consistency.So What Should You Do?
If you’re on simvastatin, lovastatin, or fluvastatin-the short-acting ones-your doctor might still suggest bedtime. But even then, if you consistently forget, switching to morning dosing with a reminder system (phone alarm, pill box, routine tied to brushing your teeth) is better than skipping doses. If you’re on atorvastatin, rosuvastatin, pitavastatin, or pravastatin? Timing doesn’t matter. Take it when it fits your life. Morning with breakfast? Fine. Evening with dinner? Fine. Bedtime? Fine. The only rule: do it every day. The American College of Cardiology’s 2022 guidelines say it plainly: “Prioritize establishing a consistent daily routine that the patient can maintain long-term.” That’s it. No magic hour. No biological imperative. Just consistency.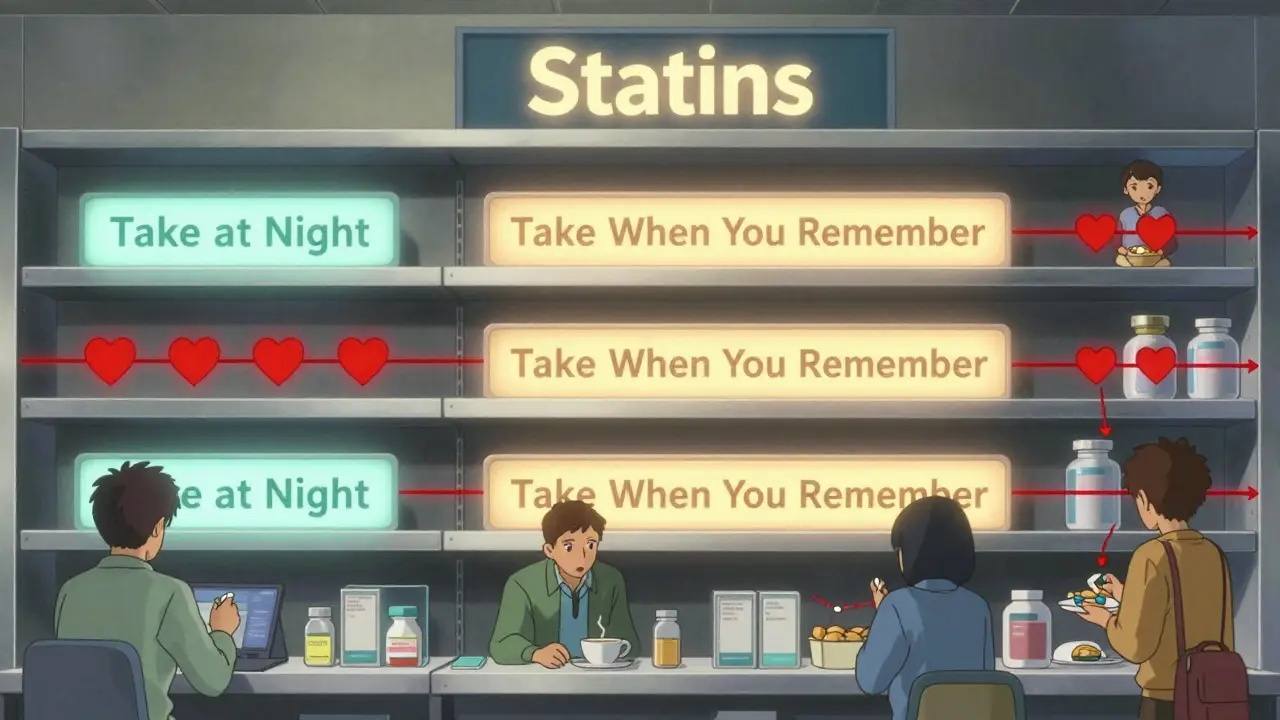
Why the Confusion Still Exists
You’ll still hear old advice floating around. Some doctors learned it in med school and never updated their practice. Some pharmacies still print “take at night” on labels. Some websites still repeat the myth. But the science has moved on. The European Medicines Agency removed timing requirements for atorvastatin and rosuvastatin in 2021. The FDA didn’t update its labels for long-acting statins because they didn’t need to-the data showed no benefit to evening dosing. The bigger shift? Prescribing patterns. In 2010, only 55% of statin prescriptions were for long-acting drugs. Now it’s 82%. That means most patients don’t even need to think about timing. And by 2030, that number is expected to hit 90%. The debate is fading-not because we don’t care, but because it’s become irrelevant for most people.Real-Life Advice
Here’s what to do right now:- If you’re on simvastatin or lovastatin: Try taking it at night. But if you forget more than once a week, talk to your doctor about switching to a long-acting statin-or move your dose to the morning with a reliable reminder.
- If you’re on atorvastatin, rosuvastatin, or pitavastatin: Take it whenever you remember. No need to change. Consistency beats clock time.
- If you’re unsure: Check your prescription. Look up the generic name. If it ends in “-vastatin,” it’s likely long-acting. If it’s simvastatin or lovastatin, timing still matters-but only if you’re consistent.
One patient told me: “I used to feel guilty for missing my night dose. Then my pharmacist said, ‘If you take it at breakfast and never miss, you’re doing better than someone who takes it at night but skips every third day.’ I haven’t looked back.”
That’s the truth. Statins work because you take them. Not because you take them at midnight.
Do I need to take my statin at night if I’m on simvastatin?
If you’re on simvastatin or lovastatin, evening dosing is theoretically better because these statins have short half-lives and peak cholesterol production happens at night. But if you consistently forget to take it at night, switching to a morning dose with a reminder system is better than missing doses. The goal is daily adherence-not perfect timing.
Can I switch my statin from night to morning?
Yes, absolutely-if you’re on a long-acting statin like atorvastatin, rosuvastatin, or pitavastatin, switching from night to morning has no impact on effectiveness. Even for short-acting statins, if you’re struggling with nighttime adherence, a morning switch is often recommended. Talk to your doctor first, but don’t assume timing is a barrier you can’t overcome.
Does taking statins at night reduce side effects?
No. Large studies analyzing millions of prescriptions show no difference in side effects like muscle pain, liver enzyme changes, or diabetes risk based on whether statins are taken in the morning or at night. Side effects are related to the drug itself and individual factors like age, activity level, and genetics-not timing.
Why do some pharmacies still say “take at night” on the label?
Many pharmacy labels haven’t been updated since older guidelines existed. Pharmacists are catching up, but the system moves slowly. If your label says “take at night” but you’re on rosuvastatin or atorvastatin, you can safely ignore it. The prescribing doctor’s instructions override the label. Always check with your provider if you’re unsure.
What if I take my statin at different times each day?
For long-acting statins (atorvastatin, rosuvastatin, etc.), occasional variation in timing won’t hurt. But for short-acting statins like simvastatin, inconsistent timing can reduce effectiveness. If you’re frequently changing your schedule, consider switching to a long-acting statin or using a daily reminder (phone alarm, pill box, habit stacking) to build consistency.

