Why Movement Matters More Than You Think
When your knees ache every morning or your hips stiffen after sitting too long, it’s easy to assume rest is the answer. But what if the real solution isn’t less movement-but better movement? Physical therapy for joint disorders isn’t about pushing through pain. It’s about rebuilding what pain has stolen: your ability to move without fear. The science is clear. For osteoarthritis, rheumatoid arthritis, and other joint conditions, structured range of motion and strengthening exercises don’t just ease symptoms-they change the disease’s course.
A 2023 review of 127 clinical trials found that patients who followed a physical therapy program saw a 37.6% drop in pain and nearly 30% improvement in daily function compared to those who didn’t. That’s not a small gain. That’s the difference between needing help to get out of a chair and doing it on your own. And it’s not just about comfort. Studies show physical therapy can delay or even prevent joint replacement surgery by years.
Range of Motion: Getting Back What You Lost
Joint stiffness isn’t just annoying-it’s dangerous. When you stop moving a joint fully, the surrounding tissues tighten, cartilage loses nutrients, and muscles weaken. That’s why range of motion (ROM) exercises are the first step in any physical therapy plan.
For knee osteoarthritis, therapists don’t just ask you to bend and straighten your leg. They use precise protocols: 3 sets of 10-15 repetitions of terminal knee extension (the last 10-15 degrees of straightening), done five days a week. The resistance? Just enough to feel tension-not pain. Pain should stay below 3 out of 10 during exercise. Too much, and you risk inflammation. Too little, and you get no progress.
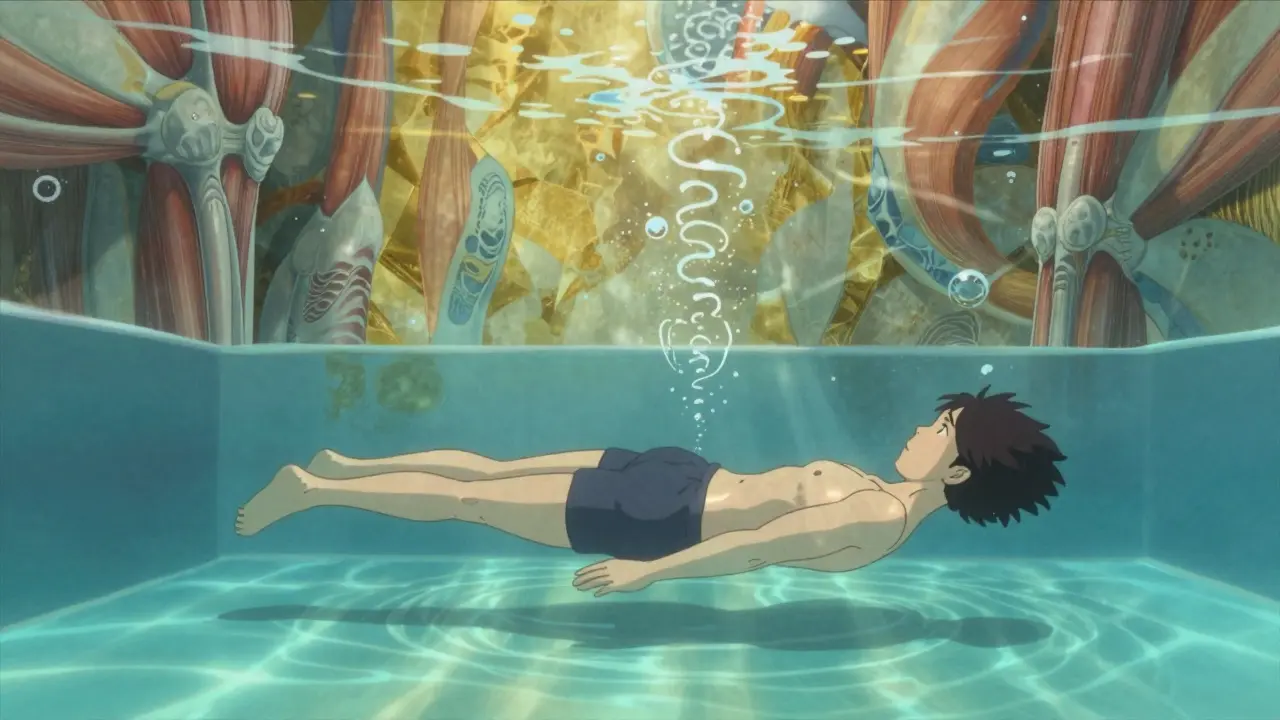
For hips, gentle circular motions and seated leg slides help restore movement. In water, the buoyancy reduces pressure while still allowing full motion. Aquatic therapy sessions, at 33-36°C (91-97°F), are especially effective for people with severe stiffness. Thirty to forty-five minutes, three times a week, can unlock mobility that land-based exercises alone can’t reach.
It’s not about how far you can stretch. It’s about consistency. One patient with knee OA told her therapist, “I didn’t think moving my knee 5 degrees more would matter.” But after six weeks, she could climb stairs without gripping the railing. That’s the power of small, daily gains.
Strengthening: Building Your Joint’s Natural Support System
Your muscles are your body’s shock absorbers. When they’re weak, your joints take the hit. Strengthening isn’t about lifting heavy weights. It’s about training your muscles to protect your joints.
For hip osteoarthritis, the 2025 JOSPT guidelines recommend hip abductor exercises using 2.5-5.0 kg resistance. Three sets of 15 reps, three times a week. That’s it. No machines. No fancy equipment. Just a resistance band or light dumbbell. The goal? To stabilize the pelvis so your hip joint doesn’t grind.
For knee OA, quadriceps strengthening is non-negotiable. Exercises like straight leg raises and seated knee extensions at 40-60% of your one-rep max (1RM) are proven to reduce pain and improve walking speed. A 2022 study found that patients who did these exercises for 12 weeks could walk 34 meters farther in six minutes-enough to get to the mailbox without stopping.
And here’s something most people don’t realize: isometric exercises-where you tighten muscles without moving the joint-are just as important, especially in the early stages. A simple quad set (tightening your thigh muscle while sitting) can be done even when movement hurts. It builds strength without stressing the joint.
When Physical Therapy Works Best (and When It Doesn’t)
Physical therapy isn’t magic. It’s science-and science has limits.
For mild to moderate osteoarthritis, studies show physical therapy delivers results equal to hip replacement surgery at the 12-month mark. One group of patients had WOMAC pain scores of 45.2 after therapy. The surgery group? 43.8. The difference? Statistically meaningless. But therapy costs a fraction of surgery and carries no risk of infection or implant failure.
But when joint space narrowing exceeds 50% on an X-ray, exercise alone won’t rebuild cartilage. That’s not a failure of therapy-it’s a sign that other options need to be considered. Physical therapy still helps, but it shifts from disease-modifying to symptom-managing.
And not all programs are equal. A 2022 study found that generic exercise plans-like “just walk more”-only helped 12-15% of patients. But when therapists used individualized programs based on your pain level, mobility, and strength? Success jumped to 65-70%.
What the Experts Say
Dr. Susan Goodman, lead author of the 2021 American College of Rheumatology guidelines, calls exercise “disease-modifying therapy.” That’s a big deal. It means movement doesn’t just mask pain-it slows joint damage. Patients who stick with their program show 23% slower cartilage loss over time.
Dr. Michael Skolnik, an orthopedic surgeon, says pre-surgery physical therapy reduces complications by 31% and shortens hospital stays by almost two days. That’s not just about comfort-it’s about safety and cost.
But there’s a warning too. Dr. Thomas Schnitzer, a leading osteoarthritis researcher, says: “Generic prescriptions yield generic results.” If your therapist gives you the same exercises they gave five other patients, you’re not getting the care you need.
Real People, Real Results
On Healthgrades, physical therapy for joint disorders has a 4.2 out of 5 rating from nearly 15,000 reviews. Most people report major improvements within eight weeks. One common milestone? “I can get up from the toilet without using my hands.”
But it’s not all smooth sailing. Over 40% of Reddit users in r/Physical_Therapy say the first two weeks hurt more than before. That’s normal. Muscles that haven’t worked in months are waking up. It’s not a sign to quit-it’s a sign you’re doing it right.
The real barrier? Access. A 2022 Arthritis Foundation survey found one-third of patients quit therapy because they couldn’t get there. Rural residents were two and a half times more likely to drop out. Insurance limits are another problem. Many plans cap visits at 10 or 12, even though Medicare data shows most patients hit their goals by session 12.
What You Can Do Right Now
You don’t need a fancy gym or expensive equipment. Start today:
- For knee stiffness: Sit in a chair. Slowly straighten one leg, hold for 5 seconds, then lower. Do 10 reps per leg, twice daily.
- For hip weakness: Stand behind a chair. Lift one leg out to the side, keeping your torso still. Lower slowly. Do 15 reps per side, three times a week.
- For general mobility: Walk for 10 minutes every day. If that’s too much, break it into three 3-minute walks.
Track your progress. Can you climb stairs without holding on? Can you stand from a chair without using your arms? Those are your real milestones.
The Future Is Personalized
Physical therapy is changing fast. In 2025, new guidelines use machine learning to predict which exercises will work best for you-based on your age, weight, X-ray results, and pain levels. Wearable sensors now let therapists monitor your form remotely, ensuring you’re doing exercises correctly even if you’re at home.
Starting in 2026, Medicare will cover maintenance therapy for chronic joint conditions. That means you won’t have to stop when you feel better-you’ll be able to keep going to stay better.
But the core hasn’t changed. It’s still about movement. Still about consistency. Still about doing the right thing, even when it’s hard.
Can physical therapy really delay or avoid joint replacement surgery?
Yes, for mild to moderate osteoarthritis. A 2023 study in Arthritis & Rheumatology found that physical therapy delivered the same functional outcomes as hip replacement at 12 months. Patients who stuck with therapy delayed surgery by an average of 2.7 years. Physical therapy strengthens the muscles around the joint, reduces inflammation, and improves movement patterns-slowing the progression of damage. It’s not a cure, but it’s a powerful delay tactic.
How often should I do range of motion exercises?
Daily. For most joint disorders, gentle range of motion should be done every day, even on days you feel stiff. The goal isn’t to push through pain, but to maintain mobility. For knee OA, therapists recommend 3 sets of 10-15 repetitions of terminal knee extension, five days a week. For hips and shoulders, 5-10 minutes of slow, controlled movements in the morning and evening helps prevent stiffness from building up.
Is it normal for my joint to hurt more at first during physical therapy?
Mild discomfort in the first 1-2 weeks is common, especially if you’ve been inactive. But sharp pain, swelling, or pain lasting more than 2 hours after exercise means you’re overdoing it. Pain should stay below 3 out of 10 during movement. If you’re hurting badly, talk to your therapist. They can adjust resistance, reduce frequency, or switch to water-based exercises. Pushing through pain isn’t progress-it’s injury.
Do I need special equipment for strengthening exercises?
No. Most effective strengthening for joint disorders uses light resistance: ankle weights, resistance bands, or even your own body weight. For hip abductor exercises, a simple loop band around your thighs works better than heavy machines. For knees, seated leg extensions with 2.5 kg ankle weights are proven to improve function. The key isn’t the tool-it’s the precision. Doing 15 reps slowly with control beats doing 50 reps fast with poor form.
Why do some physical therapy programs fail?
Most fail because they’re not personalized. A 2022 study showed generic exercise plans-like “just walk more”-only helped 12-15% of patients. But when therapists assessed your pain level, joint alignment, muscle strength, and daily habits, success jumped to 65-70%. Another common reason is lack of follow-through. Studies show you need at least 70% adherence to see results. Missing two or three sessions a week won’t cut it. Consistency beats intensity.
Can I do physical therapy at home?
Yes-especially with new telehealth tools. Starting in 2025, Medicare and private insurers began covering remotely monitored programs using wearable sensors that track your movement accuracy. If your therapist gives you a clear plan with specific reps, sets, and pain limits, you can do it at home. But you still need an initial evaluation by a licensed physical therapist to make sure you’re doing the right exercises for your condition. Don’t rely on YouTube videos alone.
Next Steps: What to Do If You’re Not Seeing Results
If you’ve been doing physical therapy for 6-8 weeks and still can’t climb stairs, stand from a chair, or walk without pain, it’s time to reassess. Ask your therapist:
- Are my exercises based on my specific joint, pain level, and mobility limits?
- Am I progressing in resistance or reps every 1-2 weeks?
- Are we tracking my progress with a validated tool like the HOOS or KOOS?
- Have we ruled out other issues like nerve compression or muscle imbalances?
If you’re in a rural area and can’t get to a clinic, ask about telehealth options. Many insurers now cover virtual sessions with movement-tracking apps. And if your insurance limits sessions, ask your therapist to give you a long-term maintenance plan-you can keep doing the core exercises on your own.
Physical therapy isn’t a quick fix. It’s a long-term investment in your body. But for joint disorders, it’s the most effective, safest, and cheapest tool we have. The question isn’t whether you can afford it. It’s whether you can afford not to try.

