After a liver transplant, the real work begins-not in the hospital, but in your daily life. The surgery was a miracle. But surviving long-term? That’s about what you do every single day after you walk out the door. Your new liver is a gift, but it’s also a target. Your body doesn’t know it’s supposed to accept it. Left unchecked, your immune system will attack it. That’s rejection. And it doesn’t always come with a siren. Sometimes, it’s just a quiet drop in energy, a slight rise in blood pressure, or a missed pill you didn’t think mattered.
What Rejection Looks Like-And What It Doesn’t
Rejection isn’t one thing. It’s three different threats, each with its own timeline and warning signs. The most dangerous kind-hyperacute rejection-happens in minutes or hours. Thankfully, modern testing makes this rare. Less than 1 in 100 transplants see this now. You won’t have to worry about it unless something went terribly wrong during surgery.
The real enemy is acute rejection. It usually shows up between one week and three months after transplant, but it can strike anytime-even years later. This is where most patients slip up. And it’s sneaky. You might feel fine. No fever. No pain. But your liver is already under attack.
Here’s what to watch for:
- Fever above 100°F (37.8°C), even if it’s just for a day
- Unexplained fatigue, like you’ve been hit by a truck
- Tenderness or swelling near your transplant site
- Nausea or loss of appetite, when you used to eat normally
- Dark urine or very little urine output
- Rapid weight gain-10 pounds or more in under 48 hours
- Jaundice (yellowing of skin or eyes)
These aren’t just "bad days." They’re red flags. If you notice even one, call your transplant team right away. Don’t wait. Don’t assume it’s a cold. Don’t think, "I’ll just wait and see." Blood tests will show if your liver enzymes or bilirubin are climbing. But waiting for symptoms to show up is like waiting for your car to catch fire before checking the oil.
Chronic rejection is slower. It creeps in over months or years. No sudden spikes. Just a gradual decline: higher blood pressure, ongoing tiredness, rising creatinine levels. It’s harder to catch. That’s why regular blood work isn’t optional-it’s your lifeline.
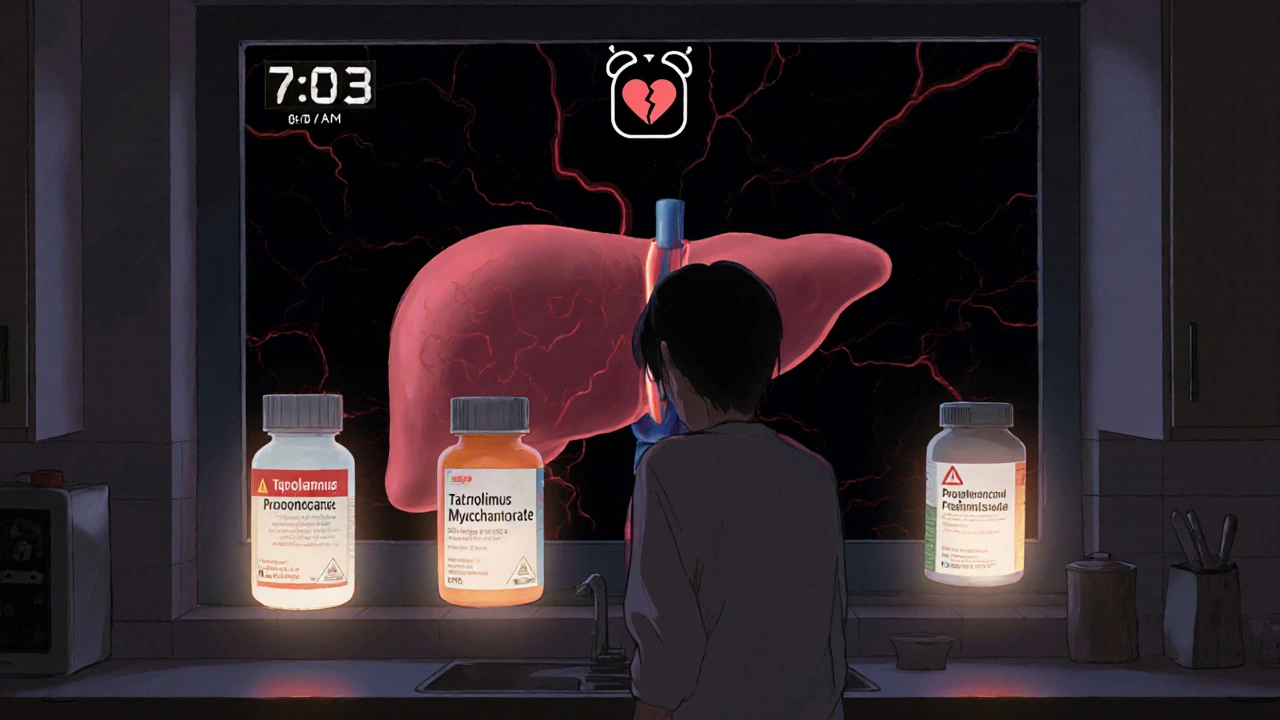
Why Taking Your Pills Isn’t Optional-It’s Survival
Your immunosuppressants aren’t vitamins. They’re life-support drugs. They keep your immune system from killing your new liver. Skip them, and you’re playing Russian roulette with your organ.
Studies show that patients who miss just 20% of their doses have three times higher risk of rejection than those who take every pill on time. And it’s not just about the pills you forget. It’s about the ones you skip because you feel fine. Or because they make you shaky. Or because they cost too much. Or because you’re tired of taking 12 pills a day.
Here’s what your typical regimen looks like:
- Calcineurin inhibitors (tacrolimus or cyclosporine)-the backbone of your therapy. Blood levels must be kept between 5-10 ng/mL in the first year.
- Antimetabolites (mycophenolate or azathioprine)-stop immune cells from multiplying.
- Corticosteroids (prednisone)-reduce inflammation. Often tapered over time, but never stopped abruptly.
Each drug has side effects. Tremors. High blood pressure. Weight gain. Diarrhea. Mood swings. It’s not easy. But here’s the truth: the side effects are manageable. Rejection is not.
One study found that patients who took less than 90% of their doses had a 23% higher chance of losing their transplant for every 10% drop in adherence. That’s not a risk. That’s a guarantee of failure.
And it’s not just about you. A 2022 report from the Scientific Registry of Transplant Recipients showed that patients who stuck to their meds had a 95% one-year survival rate. Those who didn’t? 78%. That’s a 17-point gap. That’s 17 people out of 100 who could have lived longer-if they’d taken their pills.
How to Actually Remember Your Meds (When Life Gets Busy)
You know you should take your pills. But you forget. You’re overwhelmed. You’re traveling. You’re tired. You’re angry. You’re in pain. You’re not alone.
Here’s what works, based on real data from transplant centers:
- Use a pill organizer-the kind with separate compartments for morning, noon, night. 63% of long-term survivors use one. Simple. Reliable. No batteries needed.
- Set phone alarms-three times a day, at the same time. Don’t snooze. Label them: "Tacrolimus AM," "Mycophenolate PM." A 2022 JAMA study showed this improves adherence by 37%.
- Link pills to habits-take them right after brushing your teeth, or with your morning coffee. Your brain remembers routines better than random reminders.
- Involve someone-a spouse, child, friend. Ask them to check in. A Cleveland Clinic study found family support cuts rejection risk by 28%.
- Use smart pill bottles-some now track when you open them. If you miss a dose, your pharmacist gets an alert. 35% of major U.S. centers now use these. They don’t judge. They just help.
Don’t rely on memory. Don’t hope you’ll remember. Build systems. Your liver doesn’t care if you had a bad day. It only cares if you took your medicine.

What to Do When You Can’t Afford Your Meds
Let’s be real. A year’s supply of immunosuppressants can cost $28,000 without insurance. That’s not a number. That’s a crisis.
But you’re not stuck. There are options:
- Ask your transplant center’s social worker. They know every patient assistance program, charity, and drug manufacturer discount.
- Apply for Medicaid or Medicare if you qualify. Transplant patients often get automatic eligibility.
- Check if your drug has a generic version. Tacrolimus has one now. It’s just as effective.
- Don’t split pills or skip doses to stretch your supply. That’s how grafts die.
Pharmacists at transplant centers are trained to help with this. They’ll find you savings you didn’t know existed. But you have to ask. Silence costs more than money-it costs your liver.
When You’re Not Feeling Like Yourself
It’s normal to feel different after a transplant. You’re not the same person you were before. You’re tired. You’re anxious. You’re angry. You’re grateful. You’re guilty. You feel like a burden. You feel like a miracle.
These feelings don’t make you weak. They make you human.
But depression and anxiety can sabotage your meds. If you’re losing motivation, skipping appointments, or feeling hopeless-say something. Talk to your transplant team. Ask for a counselor. Join a support group. You don’t have to carry this alone.
One patient in Wellington told me: "I missed my pills for three days because I didn’t want to face the fact that I was still sick. My doctor didn’t yell. She just said, ‘We’re here to help you live. Not just survive.’ That changed everything."

The Future Is Getting Smarter
Science isn’t standing still. In January 2023, the FDA approved the first genetic test for tacrolimus dosing-XyGlo. It looks at your DNA to predict how your body processes the drug. No more guessing. No more frequent blood draws. Just better, personalized care.
Some centers are now using the ImmuKnow assay-a blood test that measures your immune system’s activity. It tells doctors if you’re over-immunosuppressed (at risk for infection) or under-immunosuppressed (at risk for rejection). This isn’t science fiction. It’s happening now.
And then there’s the big hope: tolerance. In a recent trial, 40% of patients who got a stem cell transplant along with their kidney were able to stop all immunosuppressants after 18 months. No pills. No side effects. Just a working organ. It’s early. It’s not for everyone. But it’s real.
For now, though, the answer is still simple: take your pills. Show up for your labs. Speak up when something’s off.
What Happens If You Stop?
Let’s say you stop your meds for a week. What happens?
Your immune system wakes up. It starts attacking your liver. You might not feel it. But your liver cells are dying. Scar tissue forms. Blood flow slows. Function drops. You get sicker. You go back to the hospital. They try to reverse it with stronger drugs. Sometimes it works. Sometimes it doesn’t.
If it doesn’t? You’re back on the transplant list. But now you’re older. Sicker. Maybe you’ve had infections. Maybe your heart is damaged. Your chances of getting another liver? Lower. Your chances of surviving it? Even lower.
One transplant surgeon said it best: "We don’t fail patients in the OR. We fail them in their kitchen, in their bedroom, in their silence."
Can rejection happen years after a liver transplant?
Yes. While acute rejection most often occurs in the first few months, it can happen at any time-even 10 or more years after transplant. Chronic rejection develops slowly over time and is often linked to long-term medication non-adherence. Regular blood tests and checkups are critical, no matter how long it’s been since your surgery.
What happens if I miss one dose of my immunosuppressant?
Missing one dose occasionally won’t cause immediate rejection, but it increases your risk. The problem isn’t the single missed pill-it’s the pattern. Studies show that patients who miss even 20% of doses over time have three times higher rejection rates. If you miss a dose, take it as soon as you remember-unless it’s almost time for the next one. Never double up. Always call your transplant team for advice.
Are there natural ways to reduce rejection risk?
No. There are no herbs, supplements, or diets that can replace immunosuppressant drugs. Some supplements can actually interfere with your meds or harm your liver. Always talk to your transplant team before taking anything-even vitamins. The only proven way to prevent rejection is taking your prescribed medications exactly as directed.
How often do I need blood tests after a transplant?
In the first month, you’ll likely have blood tests weekly. Months 2-3: biweekly. After that, monthly for the first year. Once you’re stable, tests may drop to every 2-3 months. But if you feel unwell or miss doses, your team may ask for more frequent checks. Your creatinine and liver enzyme levels are your early warning system.
Can I ever stop taking immunosuppressants?
For almost all patients, lifelong immunosuppression is required. Stopping without medical supervision will cause rejection. There are rare experimental protocols-like stem cell transplants-that have allowed a small number of patients to stop meds, but these are not standard and only offered in clinical trials. Never stop your meds on your own.
What’s Next?
If you’re struggling with your meds, don’t wait until you’re in crisis. Talk to your pharmacist. Ask for a medication review. Set up reminders. Bring a loved one to your next appointment. Write down your concerns. You don’t have to be perfect. But you do have to be consistent.
Your liver didn’t just survive the surgery. It’s surviving because of you. Every pill. Every test. Every honest conversation with your care team. That’s what keeps it alive. Not luck. Not magic. Just you-showing up, day after day.