Why Your Plate Matters More Than You Think
If you’ve been told you have prediabetes, you’re not alone-nearly 1 in 3 American adults have it. And here’s the scary part: 80% of them don’t even know it. But the good news? You can stop it from becoming type 2 diabetes. Not with pills. Not with magic supplements. But with what you eat every day. The science is clear: eating the right kinds of fiber, protein, and choosing lower-glycemic foods can slash your risk by more than half. This isn’t about starving yourself or cutting out carbs entirely. It’s about making smarter swaps that actually work.
Fiber: The Silent Blood Sugar Stabilizer
Fiber doesn’t get digested. That’s why it’s so powerful. Instead of turning into sugar like other carbs, it slows down how fast your body absorbs glucose. The goal? 25 to 38 grams a day. Most people get less than half that.
Start with vegetables. Broccoli, spinach, kale, bell peppers-each serving gives you 3 to 5 grams of fiber and barely any sugar. Fill half your plate with them at every meal. That’s not a suggestion; it’s a proven strategy. People who use the plate method (half veggies, quarter protein, quarter whole grains) stick to it 27% better than those who don’t.
Swap white bread for whole grain. The ADA says at least half your grain intake should be whole. That means choosing steel-cut oats over instant, brown rice over white, and whole-wheat pasta over the regular kind. One study found that every extra 10 grams of fiber per day lowered diabetes risk by 23%. That’s like getting a free 23% discount on your future health.
Beans and lentils? They’re fiber powerhouses. A half-cup of black beans gives you 7.5 grams of fiber and 7 grams of protein. No other food does that combo so well.
Protein: The Slow-Moving Anchor
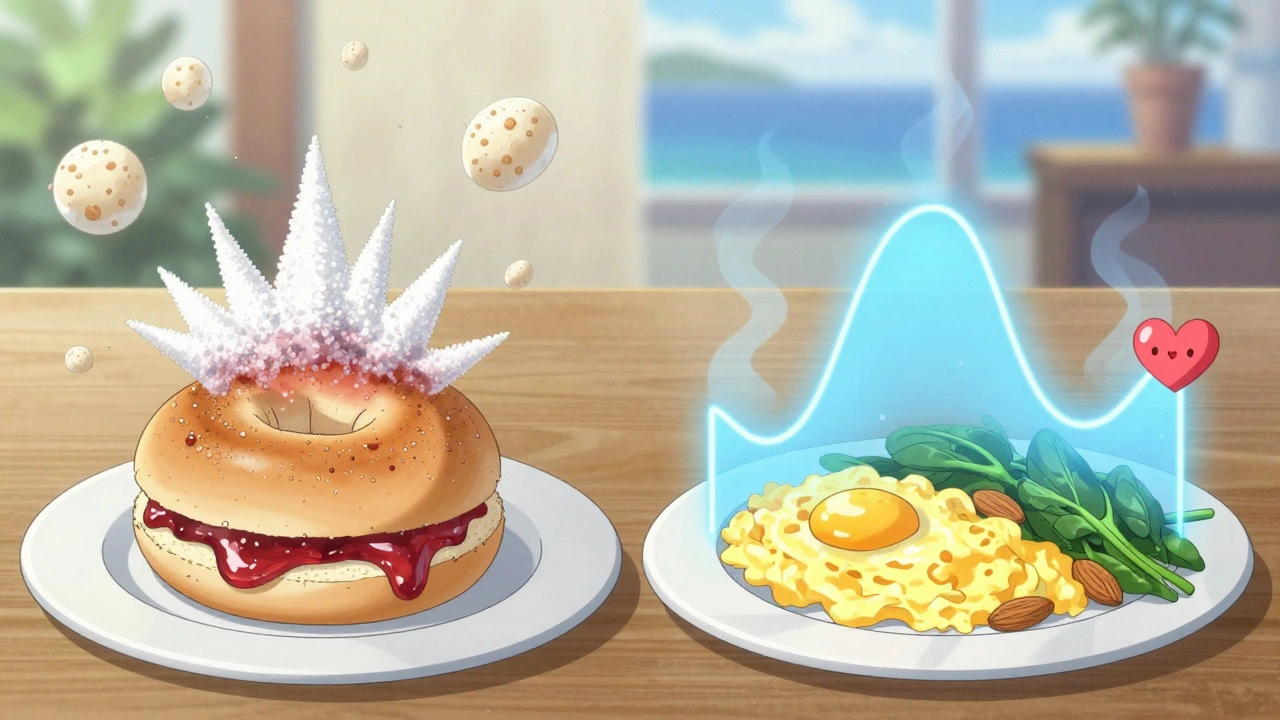
Protein doesn’t spike your blood sugar. In fact, it helps keep it steady. The key is choosing the right kinds and pairing them with carbs.
Lean meats like chicken, turkey, and fish are ideal. Eggs too. But don’t ignore plant-based proteins. Lentils, chickpeas, tofu, and edamame give you protein plus fiber-double the benefit. The IDF recommends getting 15% to 20% of your daily calories from protein. That’s about 1 to 1.2 grams per kilogram of body weight. For a 170-pound person, that’s roughly 75 to 90 grams a day.
Here’s what to avoid: red meat. A 2020 study found that eating just 100 grams of red meat a day (about the size of a deck of cards) raised diabetes risk by 20%. Processed meats like bacon and sausage? Even worse. Swap them out for grilled salmon or a tofu stir-fry.
Pair fruit with protein. Eating a banana alone? It’ll spike your sugar. Eat it with 2 tablespoons of natural peanut butter or a cup of plain Greek yogurt? The spike flattens out. Same with berries-1 cup with a handful of almonds keeps glucose under control. That’s not opinion. That’s what people on forums like Reddit are reporting: glucose levels dropping from 180 to 140 just by adding protein.
Glycemic Index: Not All Carbs Are Created Equal
The glycemic index (GI) measures how fast a food turns into sugar in your blood. High-GI foods (70+) cause quick spikes. Low-GI foods (55 or below) give you steady energy.
Here’s what to ditch: white bread (GI 75), white rice (73), and potatoes (85). These are sugar bombs in disguise. Even whole wheat bread can be high-GI if it’s finely ground. Look for stone-ground or sourdough versions-they’re lower.
Swap them for: quinoa (GI 53), sweet potatoes (44), barley (28), and legumes like lentils (32). Oats? Choose steel-cut or rolled, not instant. One person on Diabetes Daily said switching from instant to steel-cut oats dropped their morning sugar by 30 points. That’s a game-changer.
Even fruits have GI differences. Watermelon has a high GI (72), but it’s low in carbs per serving, so it’s okay in small amounts. Berries, apples, and kiwi? Low-GI and packed with fiber. Stick to 1 cup or less at a time.
The Mediterranean Diet: The Gold Standard
There’s one eating pattern that keeps coming up in every major guideline: the Mediterranean diet. It’s not a fad. It’s not restrictive. It’s simple: vegetables, fruits, beans, nuts, whole grains, olive oil, fish, and lean protein. Occasional cheese and yogurt. Rare red meat. No processed foods.
Studies show it improves blood sugar control and lowers heart disease risk. It’s not about perfection. It’s about consistency. You don’t need to eat like someone in Greece. Just borrow the principles. Have grilled salmon with roasted veggies and quinoa instead of fried chicken and fries. Swap butter for olive oil. Snack on walnuts instead of chips.
And here’s the kicker: it works. People who follow this pattern long-term reduce their diabetes risk by up to 58%. That’s the same result as the landmark Diabetes Prevention Program. No drugs. Just food.
What to Avoid (For Real This Time)
It’s not just about what to eat-it’s about what to leave out.
- Added sugars: Keep them under 10% of your daily calories. That’s about 50 grams max. A single soda has 39 grams.
- Saturated fats: Skip butter, lard, cream, coconut milk, and hard margarines. They make insulin resistance worse.
- Refined carbs: White pasta, pastries, crackers, and sugary cereals. They’re sugar with a side of nothing.
- Artificial sweeteners? They’re not the answer. Some studies link them to worse insulin response over time. Stick to water, unsweetened tea, or sparkling water with lemon.
Real People, Real Results
One woman in her 50s started eating 2 cups of non-starchy vegetables daily, swapped white rice for barley, and added a handful of almonds to her morning fruit. In 3 months, her A1c dropped from 6.1% to 5.4%. She didn’t lose weight dramatically-but her blood sugar stabilized. That’s the goal.
Another man replaced his morning bagel with scrambled eggs and spinach. His fasting sugar went from 118 to 94. He didn’t feel deprived. He felt better.
The biggest barrier? Consistency. A survey found that 42% of people struggle to eat enough vegetables every day. Portion control is tough too. 68% of prediabetics overeat carbs without realizing it.
Start small. One change at a time. Add one extra serving of veggies. Swap one refined carb for a whole grain. Add protein to your fruit. Do that for a week. Then add another. You don’t need to overhaul your life overnight. You just need to keep moving in the right direction.
What Success Looks Like
You’re not aiming for perfection. You’re aiming for progress. Here’s what to track:
- Fiber intake: 25-38 grams daily
- Protein: 15-20% of daily calories (lean or plant-based)
- Low-GI foods: Aim for average GI under 55
- Weight: Losing 5-7% of your body weight cuts diabetes risk by half
- Glucose: Fasting under 100 mg/dL, 2-hour post-meal under 140 mg/dL
These aren’t just numbers. They’re your new health markers. Track them with a simple log or app. You don’t need fancy gear. Just a notebook and honesty.
It’s Not a Diet. It’s a Lifestyle.
You won’t find a magic pill. There’s no quick fix. But there is a proven path: eat more fiber, choose lean or plant-based protein, and pick low-GI carbs. Do that consistently, and your body will thank you.
And remember: it’s not about being perfect. It’s about being persistent. One meal at a time. One swap at a time. Your future self will be glad you started today.
Can I still eat fruit if I have prediabetes?
Yes, but choose wisely. Berries, apples, kiwi, and citrus fruits are low in sugar and high in fiber. Limit portions to 1 cup at a time. Always pair fruit with a protein source like Greek yogurt, nuts, or cheese to slow sugar absorption. Avoid fruit juices-they spike blood sugar fast and lack fiber.
Is the keto diet good for prediabetes?
Keto can lower blood sugar in the short term, but it’s not sustainable for most people. It often cuts out whole grains, legumes, and fruits-foods proven to reduce diabetes risk long-term. Plus, high saturated fat intake from processed meats and cheese can worsen insulin resistance. A balanced, fiber-rich, low-GI diet works better and is easier to maintain.
How much weight do I need to lose to reverse prediabetes?
Losing just 5-7% of your body weight can cut your diabetes risk by more than half. For someone weighing 200 pounds, that’s 10 to 14 pounds. You don’t need to lose 50 pounds. Small, consistent changes in diet and activity make the biggest difference over time.
Are artificial sweeteners safe for prediabetes?
They don’t raise blood sugar directly, but research suggests they may alter gut bacteria and increase insulin resistance over time. Some studies link them to weight gain and cravings. Water, unsweetened tea, or sparkling water with lemon are safer, natural choices.
Should I take fiber supplements instead of eating fiber-rich foods?
Supplements like psyllium can help if you’re falling short, but they’re not a replacement. Whole foods give you vitamins, minerals, antioxidants, and different types of fiber that work together. Plus, eating vegetables, beans, and whole grains fills you up naturally. Supplements don’t. Aim to get most of your fiber from food.
Can I still eat bread if I have prediabetes?
Yes-but not white bread. Choose 100% whole grain, stone-ground, or sourdough bread. Look for at least 3 grams of fiber per slice. Avoid bread with added sugar, high-fructose corn syrup, or enriched flour. One slice of whole grain bread with avocado or peanut butter is a better choice than a bagel with jam.

