Generic drugs are used in 90% of all prescriptions in the U.S., yet many clinicians still hesitate to prescribe them. Why? Because they’re not fully sure they’re just as good. A 2017 study found that nearly 7 out of 10 doctors had doubts about generic medications-even though the FDA requires them to be identical in active ingredient, strength, dosage, and how they work in the body. This gap in knowledge isn’t just academic. It directly affects patients: those prescribed generics are 35% more likely to stick with their treatment than those given brand-name drugs. The problem isn’t the drugs. It’s the education.
What the FDA Actually Requires for Generics
The FDA doesn’t just approve generics because they’re cheaper. They’re approved because they’re proven to work the same way. Every generic must meet strict bioequivalence standards: the amount of drug absorbed into the bloodstream (measured by AUC) and its peak concentration (Cmax) must fall within 80% to 125% of the brand-name drug. That’s not a wide range-it’s a tight, science-backed window. If a generic falls outside those numbers, it’s rejected.
Generics must contain the same active ingredient as the brand. Same strength. Same pill, capsule, injection, or patch. The only things allowed to differ are inactive ingredients-fillers, dyes, flavors. And even those are reviewed for safety. A common myth? That generics use lower-quality manufacturing. False. The FDA inspects generic plants with the same rigor as brand-name ones. In fact, many brand-name companies make their own generics.
The FDA’s Orange Book lists every approved drug and gives it a rating. ‘A’ means therapeutically equivalent. ‘B’ means not. If a prescriber sees an ‘A’ rating, they can be confident. But too many doctors don’t know how to read it. A 2020 survey showed 45% of prescribers mistakenly believed generics must have identical inactive ingredients. They don’t. And that’s okay.
Why Clinicians Still Doubt Generics
It’s not just ignorance. It’s misinformation. A 2020 survey of 1,200 doctors found three major misconceptions:
- 45% thought generics had to have the same inactive ingredients as brands
- 38% believed generic manufacturing was less strict
- 27% thought bioequivalence meant generics could contain up to 20% less active ingredient
These aren’t minor errors. They shape prescribing habits. One resident on Reddit shared how they nearly prescribed double the dose of metoprolol because their attending said “Lopressor twice daily” without mentioning it was the same as the generic they’d already ordered. That’s not a rare mistake. It’s common.
Cardiologists and neurologists show the highest resistance. Why? Because they treat conditions where even small changes in drug levels can matter-like seizures or heart rhythm disorders. But here’s the twist: studies show no difference in outcomes between brand and generic versions of drugs like levetiracetam, metoprolol, or lisinopril. The fear is real. The evidence isn’t.
The Cost and Consequence of Not Educating Providers
Generics saved the U.S. healthcare system $2.2 trillion over the last decade. But if doctors don’t prescribe them, those savings vanish. In 2022, U.S. drug spending hit $621 billion. Generics made up only 23% of that cost-yet provided 90% of prescriptions. That’s the power of generics: same effect, far lower price.
When clinicians avoid generics, patients pay more. And when they can’t afford their meds, they skip doses. A 2020 ASPE brief showed patients on generics were 35% more likely to start and keep taking their medication. That’s not a small number. It’s the difference between someone managing their diabetes-and ending up in the hospital.
Even worse, there’s the nocebo effect. If a doctor says, “This is just the generic,” patients often report side effects they never had before. Harvard research found that when providers explicitly endorsed generic equivalence, patient-reported side effects dropped by 18%. That’s not magic. It’s trust.
What Works: Real-World Education That Changes Behavior
Not all education is equal. Sending out a PDF or hosting a one-hour webinar? That barely moves the needle. A 2021 JAMA Internal Medicine study compared two methods:
- Group 1: Received static fact sheets
- Group 2: Took part in interactive case-based sessions
At six months, Group 2 had 42% higher knowledge retention. Why? Because they practiced. They talked through real cases. They debated when to switch, how to explain it to patients, how to handle pushback.
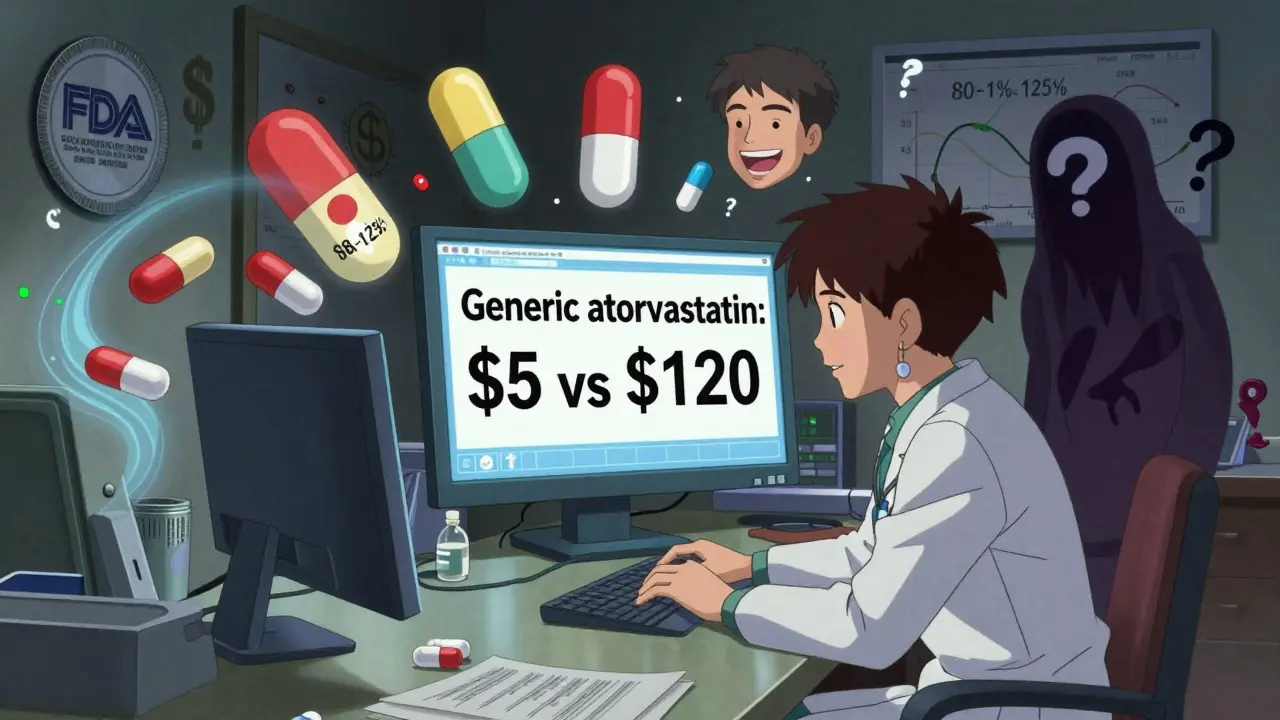
UC San Francisco Medical Center cut brand-name statin prescriptions by 37% after launching a targeted education program. They didn’t just send emails. They trained residents, held monthly case reviews, and embedded prompts into their EHR system. When a doctor typed in “Lipitor,” a pop-up appeared: “Generic atorvastatin is equivalent. Cost: $5 vs $120.” Simple. Direct. Effective.
Meanwhile, a Medicaid program in Tennessee spent $1.2 million on education and saw only 8% improvement. Why? The materials weren’t integrated into workflow. Doctors never saw them when they were prescribing. Knowledge didn’t turn into action.
How to Get Started: Practical Steps for Clinicians
You don’t need a fancy program. Start here:
- Learn the Orange Book. Go to the FDA website. Look up a drug you prescribe often. Check its rating. If it’s ‘A,’ you can confidently prescribe the generic.
- Use FDA tools. Download the Generic Drug Facts Handout and the Generic Drugs and Health Equity Handout. Keep them in your desk drawer. Review them once a month.
- Change your language. Instead of saying, “This is the generic,” say, “This is the same medication as the brand, but costs much less.”
- Ask patients. “Have you taken this before? Did it work?” You’ll be surprised how often they’ve tried generics and done fine.
- Push for EHR integration. Ask your clinic to add alerts at the point of prescribing. Show them the data: one hospital increased generic prescribing by 24% with a simple pop-up.
It takes about 6 to 8 hours of focused learning to truly understand generics. But you don’t have to do it all at once. Four 90-minute sessions over six months? That’s the sweet spot. Spaced repetition works. Memory sticks.
The Future: AI, VR, and Value-Based Care
Education is evolving. The FDA just launched virtual reality modules where doctors practice talking to simulated patients about generics. Early results? 41% increase in communication confidence.
UnitedHealthcare is using AI to track prescribing patterns. If a doctor rarely prescribes generics, they get targeted lessons-only on the drugs they use. In a 2024 pilot, that approach boosted generic prescribing by 28%.
By 2025, Medicare’s MIPS program will include generic prescribing rates as a quality metric. That means your score, your bonus, your reputation could depend on how often you choose cost-effective, equally effective generics.
Where the Education Still Falls Short
Not all drugs are created equal. Biosimilars aren’t generics. They’re complex biological drugs-like insulin or Humira. They’re not exact copies. They’re similar. And most providers don’t know the difference. A 2023 FDA survey found only 31% of clinicians could correctly explain it.
Also, state laws vary. Thirty-four states let pharmacists substitute generics without telling the prescriber. But 16 states require the doctor to write “dispense as written.” If you don’t know your state’s rules, you could accidentally block a substitution-or cause confusion.
And yes, there’s controversy. Some argue that for drugs like levothyroxine, brand-name versions are more consistent. But the FDA and most clinical guidelines say the difference is negligible. A 5.3% failure rate cited by critics? It’s been challenged by multiple studies. Don’t let outliers steer your practice.
Final Thought: Your Words Matter More Than Your Prescription
Dr. Niteesh Choudhry at Brigham and Women’s Hospital put it simply: “Provider endorsement is the single strongest predictor of patient acceptance of generics.” If you say it’s safe, patients believe it. If you hesitate, they doubt it. Even if the drug is perfect.
You don’t need to be a pharmacologist. You just need to know the facts. And then communicate them clearly. Because when you do, you’re not just prescribing a pill. You’re giving someone a chance to stay healthy without going broke.
Why do some doctors refuse to prescribe generics even when they’re approved?
Many doctors were trained during a time when generics were less common and less trusted. They learned brand names first and may not have received updated training on bioequivalence standards. Some also confuse generics with biosimilars or believe inactive ingredients affect efficacy. Misinformation, lack of exposure to data, and habit play big roles. Studies show that when doctors receive interactive education, their confidence and prescribing rates improve significantly.
Are generics as safe as brand-name drugs?
Yes. The FDA requires generics to have the same active ingredient, strength, dosage form, and route of administration as the brand. They must also meet strict bioequivalence standards-absorbing into the bloodstream at the same rate and extent. Manufacturing facilities for generics are inspected just as often as brand-name ones. The FDA has found no consistent difference in safety or effectiveness between approved generics and their brand-name counterparts.
Can pharmacists substitute a generic without the doctor’s permission?
It depends on the state. Thirty-four states allow pharmacists to substitute a generic drug without notifying the prescriber, as long as the drug has an ‘A’ rating in the FDA’s Orange Book. Sixteen states require the prescriber to write “dispense as written” on the prescription to prevent substitution. Always check your state’s pharmacy laws, and consider adding this note to prescriptions if you want to prevent substitution.
How can I learn more about generic drugs and their approval process?
Start with the FDA’s Generic Drugs Stakeholder Toolkit, which includes downloadable handouts, videos, and interactive tools. The FDA’s Orange Book is the official source for therapeutic equivalence ratings. The Generic Pharmaceutical Association (GPhA) also offers free educational modules. For deeper learning, look into accredited CME courses on therapeutic substitution and bioequivalence. Many academic medical centers now include this in residency training.
Do generics cause more side effects than brand-name drugs?
No. There is no evidence that approved generics cause more side effects. Any perceived increase is often due to the nocebo effect-when patients expect side effects because they believe the drug is inferior. Studies show that when clinicians confidently endorse generic equivalence, patient-reported side effects drop by up to 18%. The active ingredient is identical; the body responds the same way.
Is there a difference between generic and brand-name drugs for chronic conditions like hypertension or diabetes?
Multiple large-scale studies have compared outcomes for generics versus brand-name drugs in chronic conditions like hypertension, diabetes, and high cholesterol. No significant differences in effectiveness, hospitalization rates, or mortality have been found. For example, generic atorvastatin works just as well as Lipitor. Generic metformin is equally effective as Glucophage. The key is consistent use-generics help patients afford long-term treatment, which improves outcomes.