More than 1 in 10 adults over 80 in the U.S. are taking prescription sleep pills. That’s not just common-it’s alarming. These drugs might help you fall asleep tonight, but what happens when you wake up tomorrow? Or next month? Or when you try to quit?
Sleep medications aren’t harmless quick fixes. They come with real risks: memory lapses, next-day grogginess that feels like a hangover, even sleepwalking or driving while unconscious. And once you start, it’s hard to stop. Many people don’t realize they’re already dependent until they try to quit-and then can’t sleep at all.
What You’re Really Taking
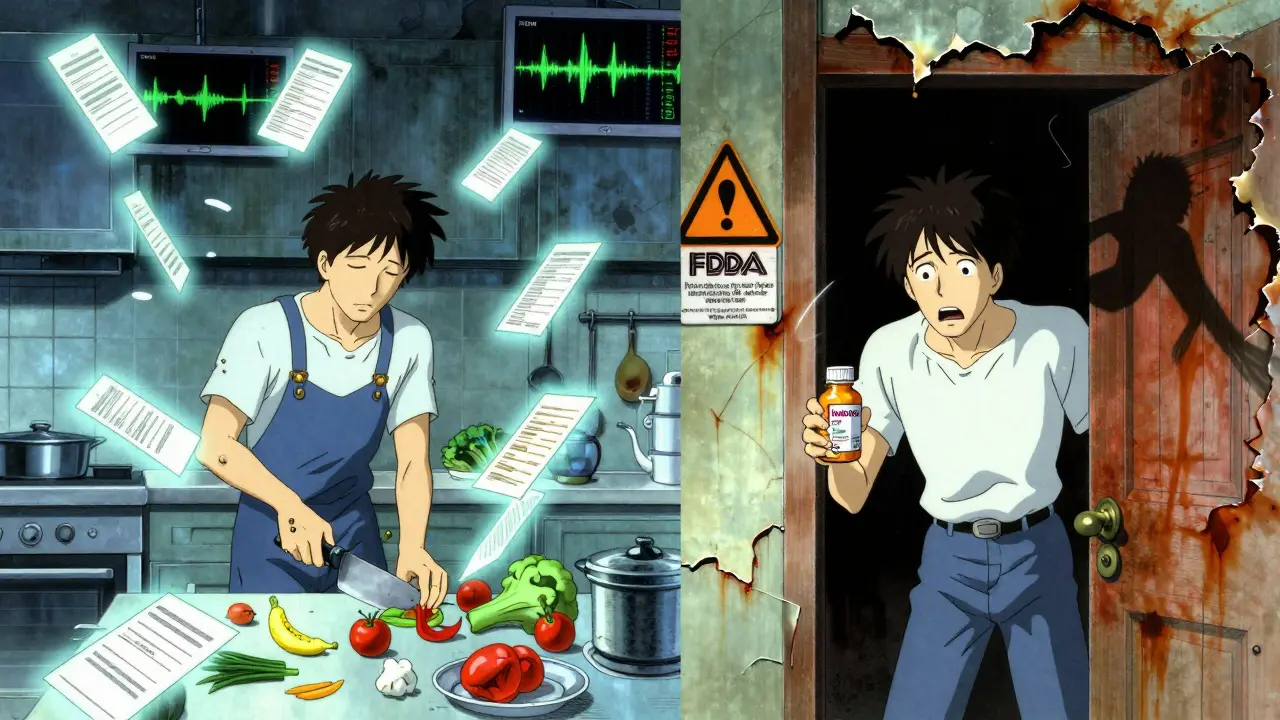
Sleep meds fall into a few main groups, each with different risks. The most common are the Z-drugs: zolpidem (Ambien), eszopiclone (Lunesta), and zaleplon (Sonata). These were marketed as safer than older drugs, but they’re not. They still target the same brain receptors, and they still cause next-day drowsiness in about 1 in 4 users. The FDA even lowered the starting dose for women in 2019 because so many were still impaired the next morning.
Benzodiazepines like lorazepam and diazepam are older, cheaper, and even riskier. They’re not even approved for long-term insomnia anymore, but doctors still prescribe them. Why? Because they work fast. But they carry a 33% chance of dependence after just six weeks. That’s not a side effect-it’s a feature of how they change your brain.
Then there are the off-label options. Trazodone, an antidepressant, is one of the most prescribed sleep aids in the U.S.-even though it was never meant for insomnia. It costs less than $10 a month, but it can cause painful, prolonged erections (priapism) in rare cases. Doxepin, sold as Silenor, helps with staying asleep but can mess with your heart rhythm at higher doses. And don’t forget the OTC stuff: diphenhydramine (Benadryl) and doxylamine (Unisom). These are antihistamines. They make you drowsy, yes-but they also block a brain chemical called acetylcholine. Long-term use? That’s linked to a 54% higher risk of dementia, according to JAMA Internal Medicine.
The Hidden Dangers
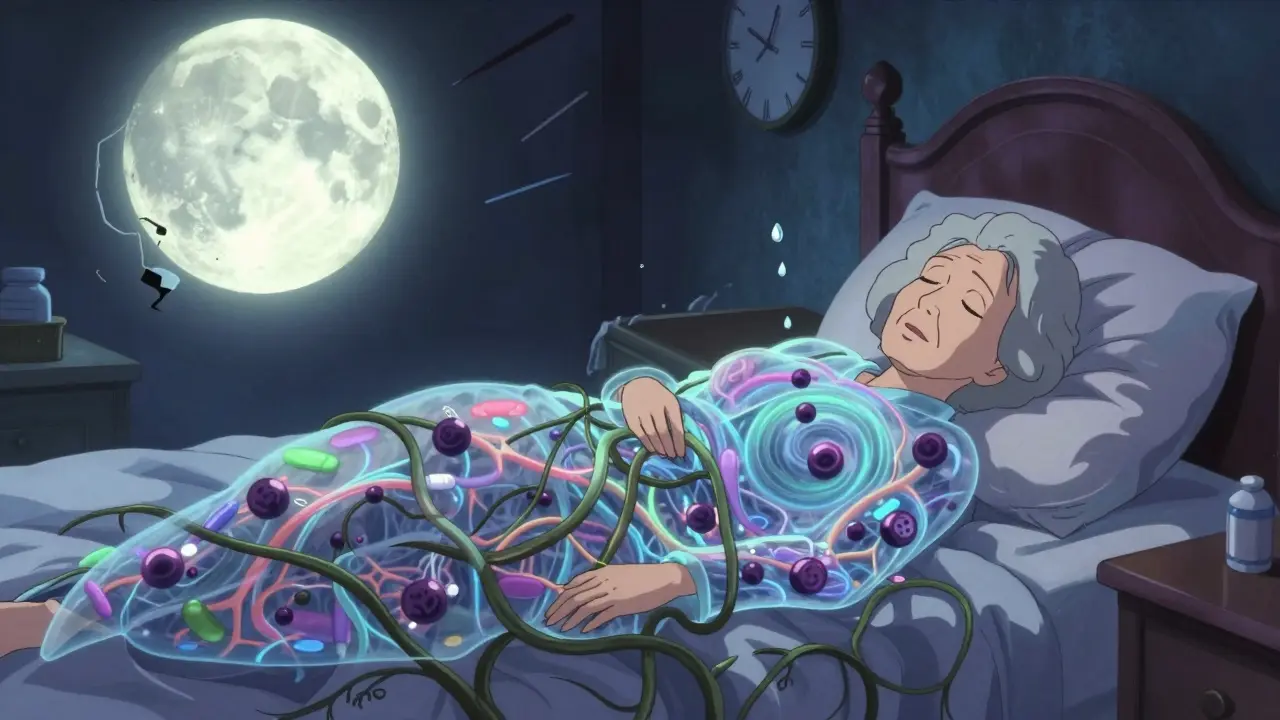
You think you’re just tired. You take a pill. You sleep. But your brain doesn’t sleep the same way. These drugs don’t restore natural sleep cycles. They suppress them. That means less deep sleep, less REM sleep-the kind your brain needs to reset. You wake up feeling like you didn’t rest at all, even if you were out for eight hours.
The next-day fog isn’t just annoying. It’s dangerous. Studies show the mental slowdown from these pills is like having a blood alcohol level of 0.05% to 0.08%. That’s legally drunk in many places. People on these meds are more likely to fall, get into car crashes, or make mistakes at work. For older adults, the risk of breaking a hip from a fall jumps by 50-60%. The American Geriatrics Society says these drugs should be avoided entirely in people over 65.
And then there’s the weird stuff. Sleepwalking. Sleep-eating. Sleep-driving. The FDA has received hundreds of reports of people doing complex tasks while half-asleep after taking zolpidem. One woman drove 17 miles to her ex’s house while asleep. Another cooked a full meal and didn’t remember it. These aren’t rare. They happen in about 1 in 200 users. And if you’re on a higher dose, or mixing with alcohol, the risk triples.
Why It’s So Hard to Quit
Dependence doesn’t always mean you’re hoarding pills or chasing highs. It means your body has adapted. You need the drug just to feel normal. When you stop, your brain goes into overdrive. You get rebound insomnia-worse than before you started. That’s why so many people stay on them for years.
One Reddit user wrote: “After six months of nightly Ambien, I tried to quit. Couldn’t sleep for three nights. Ended up right back on it.” That’s the cycle. You don’t feel addicted. You feel like you’re just managing a medical problem. But the truth? Your brain forgot how to sleep on its own.
Stopping cold turkey is risky. Withdrawal can trigger anxiety, tremors, seizures, or even psychosis. The smart way is to taper slowly-cutting your dose by 25% every two weeks. But even then, 40% of people need extra help. That’s why doctors should never hand out a 30-day script and call it a day. They need to plan the exit before they write the prescription.
What Actually Works Long-Term
There’s a better way. It’s called CBT-I-Cognitive Behavioral Therapy for Insomnia. It’s not a pill. It’s a structured program that teaches you how to fix the thoughts and habits keeping you awake. And it works better than any drug.
Studies show CBT-I helps 70-80% of people. Not just for a few weeks-years. It doesn’t just help you sleep more. It helps you sleep better. You learn to associate your bed with sleep, not stress. You stop racing your mind at night. You reset your internal clock. And you do it without chemicals.
It’s not easy. It takes time. You have to track your sleep, limit time in bed, challenge negative thoughts. Some people quit after two weeks because it feels hard. But those who stick with it? 78% say their results last longer than any medication ever did.
And now, you don’t even need to see a therapist in person. The FDA approved the first digital CBT-I app, Somryst, in 2020. It’s prescription-only, covered by some insurers, and in clinical trials, it helped 60% of users achieve full remission. No pills. No side effects. Just your phone and a few minutes a day.
New Options on the Horizon
There’s also a new class of drugs called orexin receptor antagonists. Quviviq (daridorexant), approved in 2022, works differently. Instead of sedating your brain, it blocks the chemical that keeps you awake. The result? Better sleep without the next-day grogginess. In trials, users reported 2.1 on a 10-point impairment scale-compared to 3.8 for zolpidem. That’s a big deal.
But even these aren’t magic. They’re still new. Long-term data is limited. And they cost $500+ a month. They’re not for everyone. But they show the direction things are heading: safer, smarter, more targeted sleep treatments-not just stronger sedatives.
What You Should Do Now
If you’re on a sleep med right now, don’t panic. But don’t ignore the risks either.
Ask yourself: Have I been on this for more than 4 weeks? Do I feel anxious if I miss a dose? Have I ever woken up not remembering what I did the night before? If you answered yes to any of those, it’s time to talk to your doctor-not about getting more pills, but about getting off them.
Here’s what to ask:
- Is this the shortest possible prescription?
- Have you considered CBT-I first?
- What’s the plan if I want to stop?
- Am I on the lowest effective dose?
- Are there any non-drug options I haven’t tried?
If your doctor pushes back, ask for a referral to a sleep specialist. Most major health systems now require proof that CBT-I was tried before approving long-term sleep med prescriptions. You have a right to safer care.
And if you’re thinking about starting one? Don’t. Try CBT-I first. Even if you think you don’t have time. Even if you think pills are faster. The data doesn’t lie: behavioral therapy gives you back your natural sleep-and keeps it.
Frequently Asked Questions
Can sleep medications cause dementia?
Yes, certain over-the-counter sleep aids containing antihistamines like diphenhydramine and doxylamine are linked to a 54% higher risk of dementia with long-term use, according to a study in JAMA Internal Medicine. These drugs block acetylcholine, a key brain chemical for memory. Prescription Z-drugs and benzodiazepines don’t have the same direct link, but they still impair cognitive function over time, especially in older adults.
Is melatonin safer than prescription sleep pills?
Melatonin is generally safer than prescription sleep meds because it doesn’t sedate your brain-it just signals that it’s time to sleep. Most users report no next-day grogginess. But it’s not a cure for chronic insomnia. It works best for circadian rhythm issues, like jet lag or shift work. It’s not regulated like a drug, so doses vary widely between brands. Stick to 0.3-1 mg, not the 5-10 mg pills you see on shelves.
How long can I safely take Ambien or Lunesta?
The American Academy of Sleep Medicine recommends no more than 2-5 weeks of continuous use. After that, effectiveness drops, and dependence risk rises. Many doctors prescribe longer because patients report they “need it,” but that’s a sign of tolerance-not medical necessity. If you’re still using it after a month, you should be working with a sleep specialist on a taper plan and behavioral alternatives.
Can I mix sleep meds with alcohol?
Never. Mixing alcohol with sleep medications triples your risk of overdose. Both depress your central nervous system. Together, they can shut down your breathing. Even a single drink with a Z-drug can cause dangerous drowsiness, memory blackouts, or loss of coordination. The NIH says this combination increases fatal overdose risk by 300%.
What’s the best alternative to sleeping pills?
Cognitive Behavioral Therapy for Insomnia (CBT-I) is the gold standard. It’s more effective than any drug for long-term results, with no side effects. Digital versions like Somryst are FDA-approved and covered by some insurers. Other proven alternatives include sleep restriction therapy, stimulus control, mindfulness meditation, and improving sleep hygiene-like keeping a consistent bedtime, avoiding screens before bed, and making your room cool and dark.