Most people don’t realize how quietly type 2 diabetes creeps in. No sudden pain. No dramatic warning. Just a slow fade-constant tiredness, always thirsty, cuts that won’t heal. By the time many people get tested, their blood sugar has been high for years. And that’s the problem: type 2 diabetes isn’t just about sugar. It’s about your body losing its ability to use insulin properly, and if left unchecked, it can damage your heart, kidneys, nerves, and eyes long before you feel it.
What Actually Happens in Type 2 Diabetes?
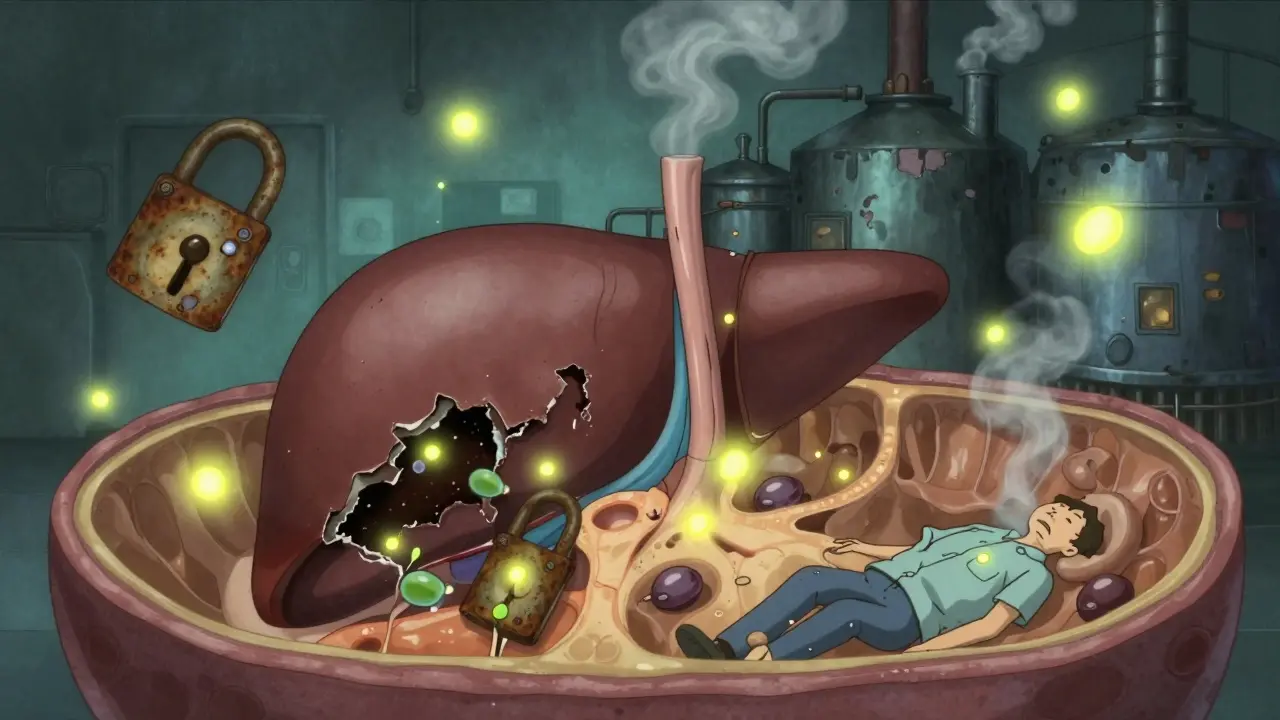
Your body breaks down food into glucose, the fuel your cells need. Insulin, a hormone made by your pancreas, acts like a key that unlocks your cells so glucose can get inside. In type 2 diabetes, those cell locks start to rust. Your muscles, fat, and liver stop responding to insulin-this is called insulin resistance. At first, your pancreas tries to compensate by pumping out more insulin. But over time, it gets worn out. By the time you’re diagnosed, you’ve already lost about half your insulin-making capacity, and it keeps declining.
This isn’t just a “sugar problem.” It’s a metabolic breakdown. The longer your blood sugar stays high, the more damage it does. That’s why so many people only find out they have it after a heart attack, kidney test, or foot ulcer. The disease doesn’t shout-it whispers for years.
What Are the Real Symptoms?
Some symptoms are obvious. Others? You might brush them off as stress, aging, or just being “out of shape.” Here’s what actually shows up in real patients:
- Constant thirst and frequent urination: High blood sugar pulls water from your tissues. Your kidneys work overtime to flush it out, leaving you dehydrated and constantly heading to the bathroom-even at night.
- Unexplained weight loss: Even if you’re eating more, your body can’t use glucose for energy. So it starts breaking down muscle and fat instead. This isn’t the kind of weight loss you want.
- Extreme fatigue: Your cells are starving for fuel, even though there’s plenty of glucose in your blood. It’s like having a full gas tank but a broken engine.
- Blurred vision: High glucose swells the lenses in your eyes. It’s often the first sign people notice when they can’t read their phone screen clearly.
- Slow-healing cuts or infections: High sugar weakens your immune system and damages blood vessels. A small scrape can turn into an ulcer. Fungal infections in the groin or feet are common.
- Tingling or numbness in hands or feet: Nerve damage from high sugar starts subtly-maybe just a pins-and-needles feeling in your toes. Left alone, it can lead to serious foot problems.
- Dark, velvety patches on skin: Called acanthosis nigricans, this shows up on the neck, armpits, or groin. It’s not dirt. It’s a visible sign of insulin resistance.
And here’s the scary part: 1 in 5 people with type 2 diabetes have no symptoms at all. They’re diagnosed during a routine blood test. That’s why getting checked-especially if you’re overweight, over 45, or have a family history-isn’t optional. It’s life-saving.
Why Do People Get Type 2 Diabetes?
It’s not just “eating too much sugar.” That’s a myth. The real causes are a mix of things you can control and things you can’t.
Obesity is the biggest driver. People with a BMI over 30 are 80 times more likely to develop type 2 diabetes than those with a BMI under 22. Fat tissue, especially around the belly, releases chemicals that interfere with insulin. Losing even 5-10% of your body weight can dramatically improve insulin sensitivity.
Inactivity makes it worse. Muscle uses glucose. If you don’t move, your muscles don’t need glucose. Your body stores it as fat instead. People who sit more than 8 hours a day have a 90% higher risk of developing diabetes than those who move regularly.
Genetics matter. If one of your parents has type 2 diabetes, your risk goes up by 40%. If both have it, your risk jumps to 70%. Over 400 genes are linked to diabetes risk. But genes don’t decide your fate-they just load the gun. Lifestyle pulls the trigger.
Some groups are at higher risk. Native Americans, African Americans, Hispanic/Latino Americans, and Asian Americans develop type 2 diabetes at much higher rates than non-Hispanic White Americans. This isn’t about biology alone-it’s about access to healthy food, safe places to exercise, and healthcare.
Age is a factor-but not the whole story. While most diagnoses happen after 45, more and more teens and young adults are getting it. In the U.S., over 287,000 people under 20 now live with type 2 diabetes. That’s a shocking shift from just 20 years ago.

What Happens If It’s Not Managed?
Uncontrolled type 2 diabetes doesn’t just make you feel bad. It silently destroys your body.
- Heart disease: People with diabetes are 2 to 4 times more likely to have a heart attack or stroke. In fact, 65-80% of deaths in people with diabetes are due to cardiovascular problems.
- Nerve damage (neuropathy): After 10 years, 60-70% of people with diabetes develop nerve damage. This leads to numb feet, burning pain, and a loss of sensation. That’s why foot ulcers happen-people don’t feel the injury until it’s infected.
- Foot amputations: 1 in 5 people with diabetic foot ulcers will need an amputation. Most are preventable with regular foot checks and good blood sugar control.
- Kidney failure: Type 2 diabetes causes 44% of new cases of kidney failure in the U.S. That means dialysis or a transplant.
- Eye damage: Diabetic retinopathy affects nearly 30% of adults with diabetes. It’s the leading cause of blindness in working-age adults.
- Brain health: There’s growing evidence that type 2 diabetes increases Alzheimer’s risk by 2 to 3 times. Some scientists now call Alzheimer’s “type 3 diabetes” because of how insulin resistance affects the brain.
- Depression: One in four people with diabetes also has depression. And depression makes diabetes harder to manage-creating a dangerous cycle.
The damage isn’t sudden. It’s cumulative. But the good news? You can stop it-or even reverse it-if you act early.
How to Manage Type 2 Diabetes-For Real
Management isn’t about pills. It’s about changing how you live. Medication helps, but it doesn’t fix the root problem. Here’s what actually works:
1. Food Is Medicine
Forget “diabetic diets.” You don’t need special foods. You need real food. Focus on:
- Vegetables (especially leafy greens)
- Lean proteins (chicken, fish, tofu, legumes)
- Whole grains (oats, quinoa, brown rice)
- Healthy fats (avocado, nuts, olive oil)
- Water, tea, black coffee
Avoid: sugary drinks, white bread, pastries, fried foods, processed snacks. These spike blood sugar fast and keep your insulin levels high.
One powerful approach: the total diet replacement method. In the DIALECT trial, 46% of people with type 2 diabetes for less than 6 years went into remission after following a strict 800-calorie liquid diet for 3-5 months, then slowly adding back real food. They didn’t need medication anymore. It’s hard-but it works.
2. Move More-Even a Little
You don’t need to run marathons. Walking 30 minutes a day, five days a week, cuts your diabetes risk by 58% if you’re prediabetic. Strength training twice a week helps too-muscle burns glucose even when you’re sitting.
Try this: Park farther away. Take the stairs. Walk after dinner. Stand up every hour. Small moves add up.
3. Medications That Work
Metformin is still the first-line drug. It lowers blood sugar, helps with weight loss, and is safe for most people. It cuts HbA1c by 1-2%.
Newer drugs are game-changers:
- GLP-1 agonists (like semaglutide, tirzepatide): Lower blood sugar, help you lose 3-15 kg, and protect your heart. Tirzepatide (Mounjaro) is now approved for type 2 diabetes and can lower HbA1c by up to 2.3%.
- SGLT2 inhibitors (like empagliflozin): Make your kidneys flush out extra sugar. They help your heart and kidneys, and you lose 2-3 kg.
These aren’t magic pills. But when paired with lifestyle changes, they’re powerful tools.
4. Monitor Your Blood Sugar
Testing isn’t about guilt. It’s about feedback. If you’re on insulin or newer drugs, checking your levels helps you see what foods spike you and what doesn’t.
Continuous glucose monitors (CGMs) are now available for type 2 diabetes. They show real-time trends-not just a number. In 2022, Medicare expanded coverage, and usage jumped from 1.2% to 12.7% in just five years. That’s progress.
5. Sleep and Stress Matter
Not enough sleep? High stress? Both raise cortisol, which raises blood sugar. Aim for 7-8 hours. Practice breathing, walking, or meditation. Your pancreas will thank you.

Can Type 2 Diabetes Be Reversed?
Yes. But “reversed” doesn’t mean cured. It means your blood sugar is normal without medication. You’re still at risk if you go back to old habits.
Studies show remission is possible if:
- You’ve had diabetes for less than 6 years
- You lose 10-15% of your body weight
- You stick with healthy eating and movement
The UKPDS study showed that early, intensive control of blood sugar leads to benefits that last for over 10 years-even after you stop the strict regimen. That’s called the “legacy effect.” The earlier you act, the longer the protection lasts.
What’s Next?
Technology is changing the game. Hybrid closed-loop systems (like the MiniMed 780G) now help type 2 patients maintain healthy blood sugar levels with less effort. The NIH’s All of Us program is studying why diabetes hits some groups harder-and how to fix it.
But the biggest challenge isn’t science. It’s access. Healthy food isn’t cheap. Safe places to walk don’t exist everywhere. Insurance doesn’t always cover CGMs or GLP-1 drugs. And stigma still makes people feel ashamed.
Managing type 2 diabetes isn’t a solo mission. It’s about community, support, and systems that make healthy choices easier.
You don’t have to be perfect. You just have to keep moving forward. One meal. One walk. One check-up at a time.